minimal invasive spine surgery
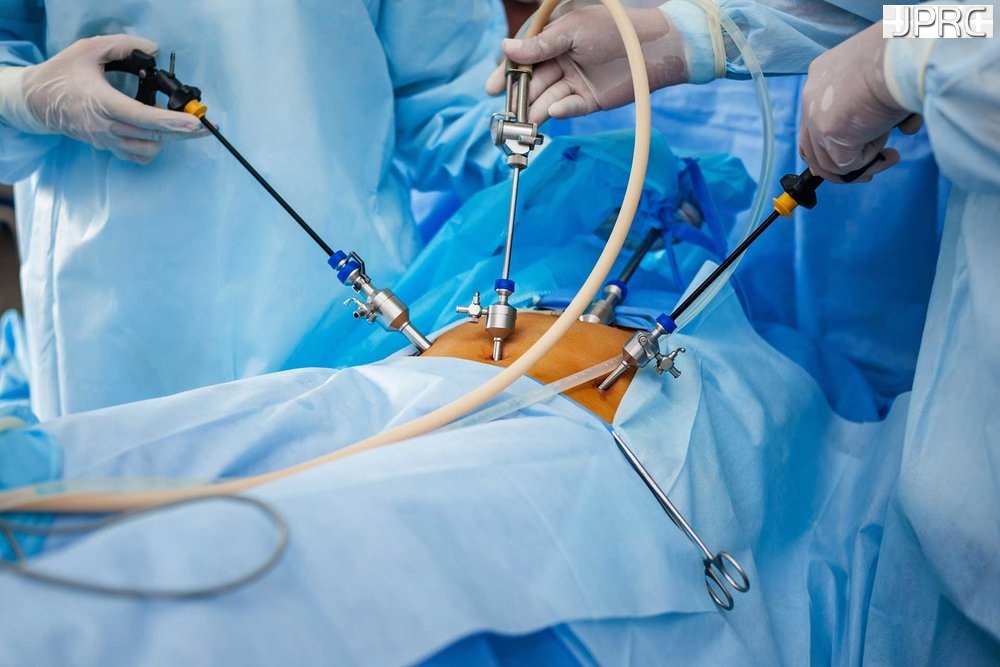
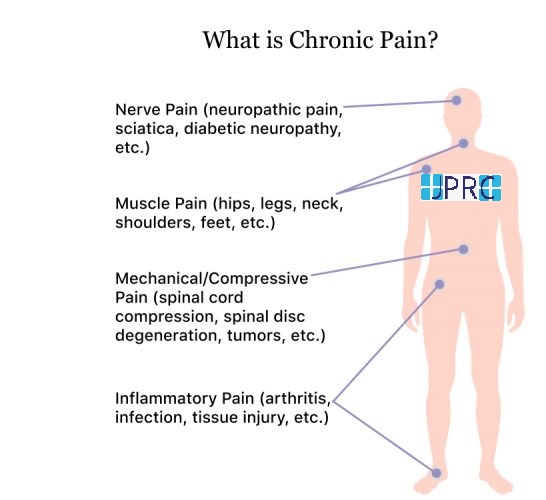
Minimally invasive spine surgery (MISS) is an alternative to traditional open surgical procedures performed to treat different spinal disorders, such as degenerative disc disease, herniated disc, scoliosis, and spinal stenosis. Spine surgery performed minimally invasively offers many potential benefits, such as small incisions, less cutting through soft tissues (eg, ligaments, muscles), outpatient options, less post-operative pain, and faster recovery.
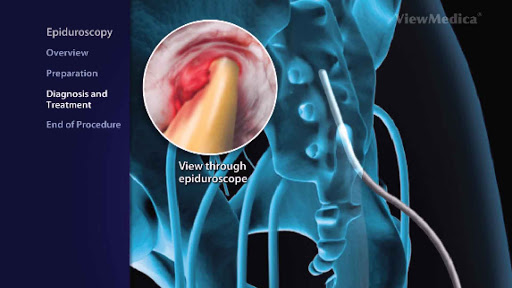
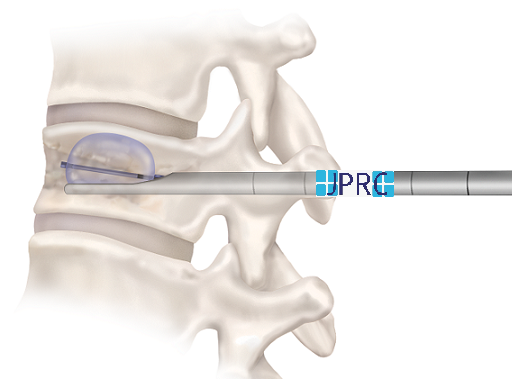
Some types of minimally invasive spine surgery involve using an endoscope and tubular retractors that help reduce soft tissue injury and post-operative pain.
Common Spine Surgery Goals
Whether spine surgery is performed open or minimally invasively, two main goals remain the same.
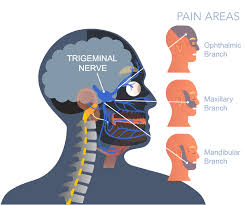
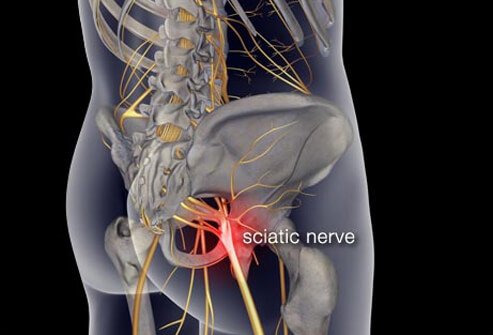
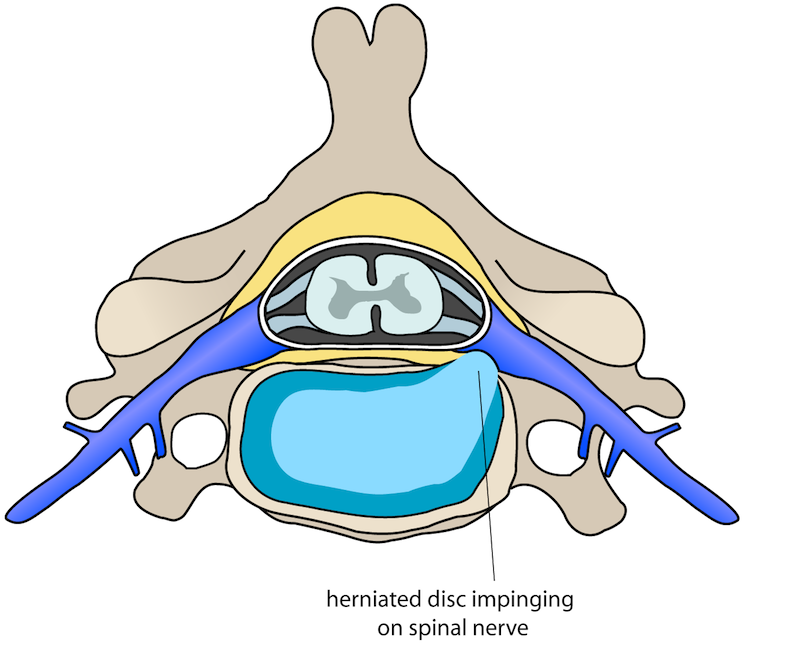
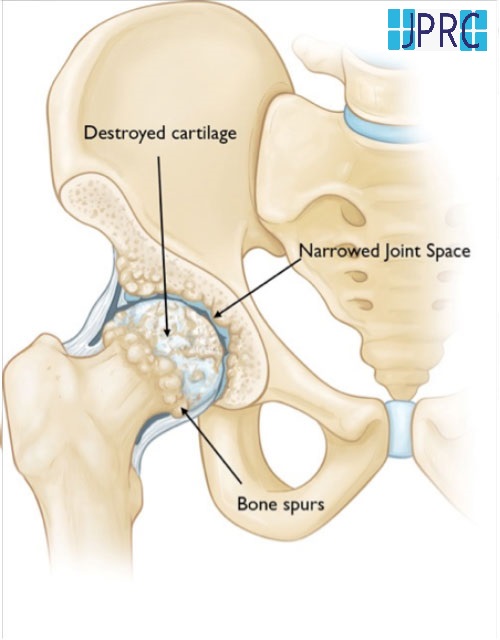
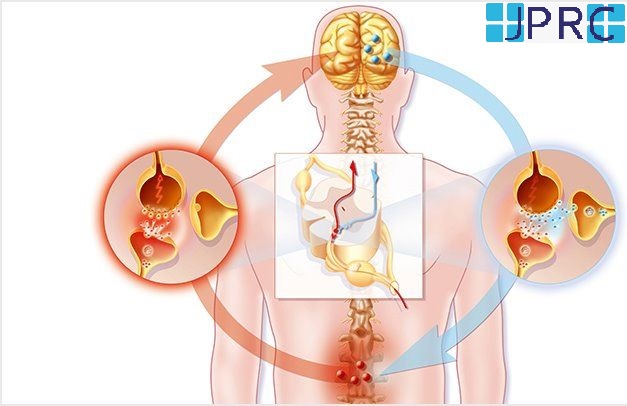
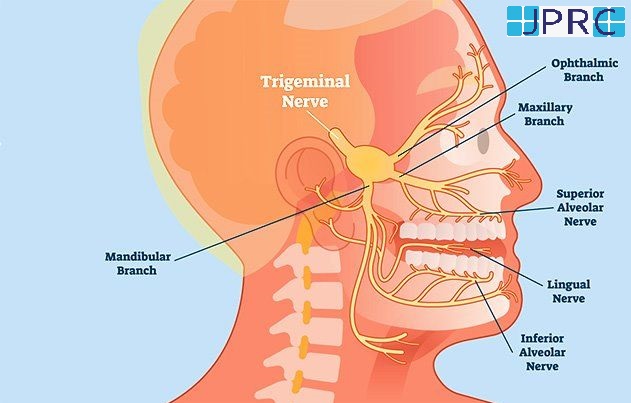
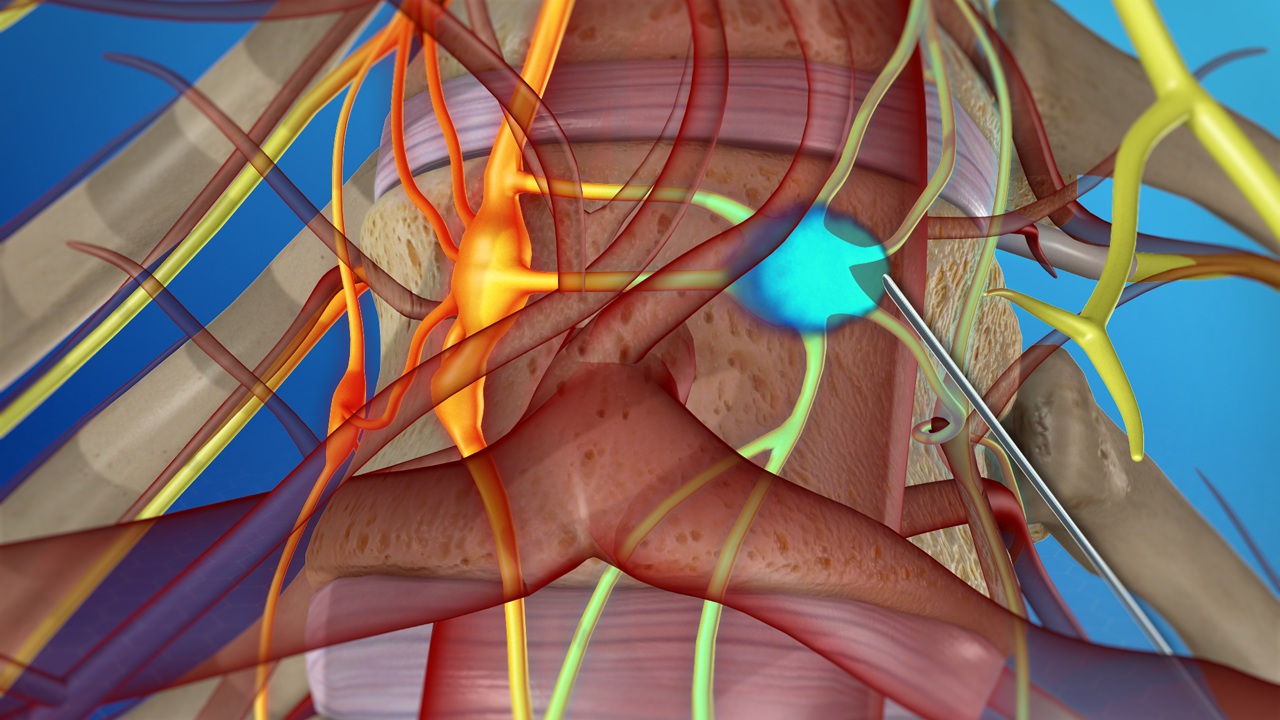
#1. Decompression: Spinal decompression involves removing tissue that is compressing nerve structures, such as a spinal nerve root and/or the spinal cord. Bone spurs and/or fragments from a herniated disc are examples of tissues that can cause neural compression.
#2. Stabilization: Abnormal movement of one or more levels or segments of the spine can cause back or neck pain. Surgical procedures that stabilize and stop the movement of the spine involve spinal instrumentation and fusion.
Minimally Invasive Spine Surgery Techniques
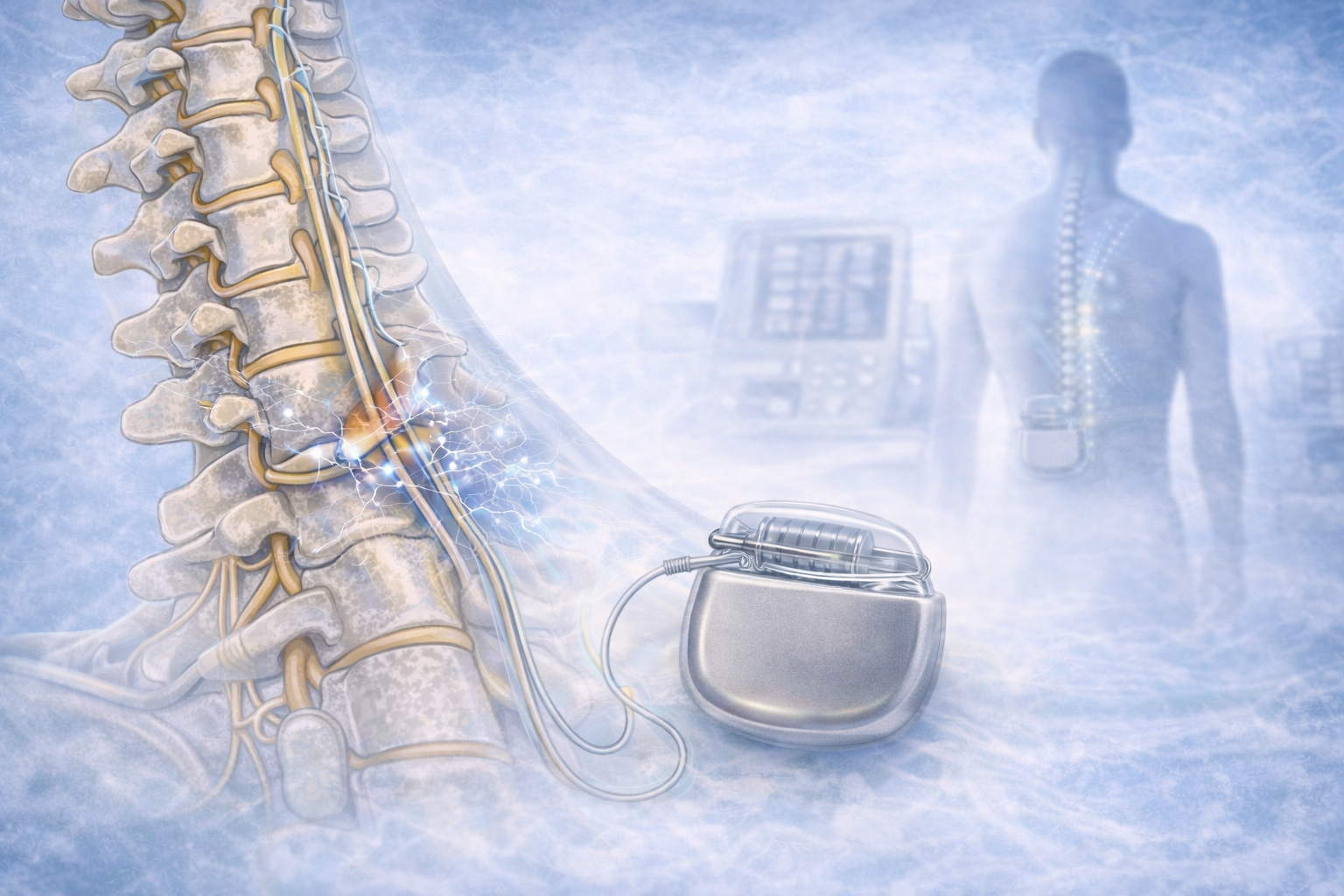
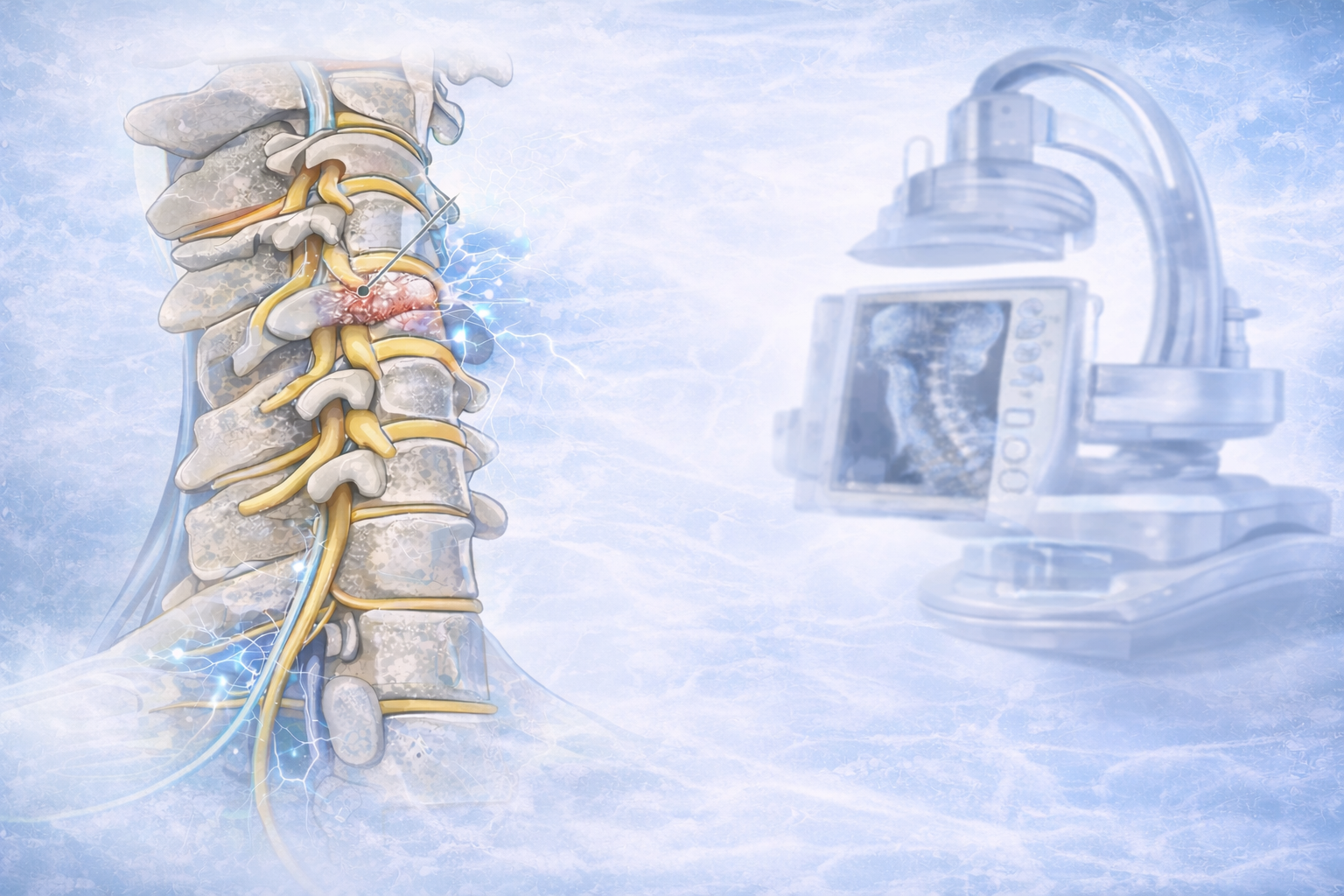
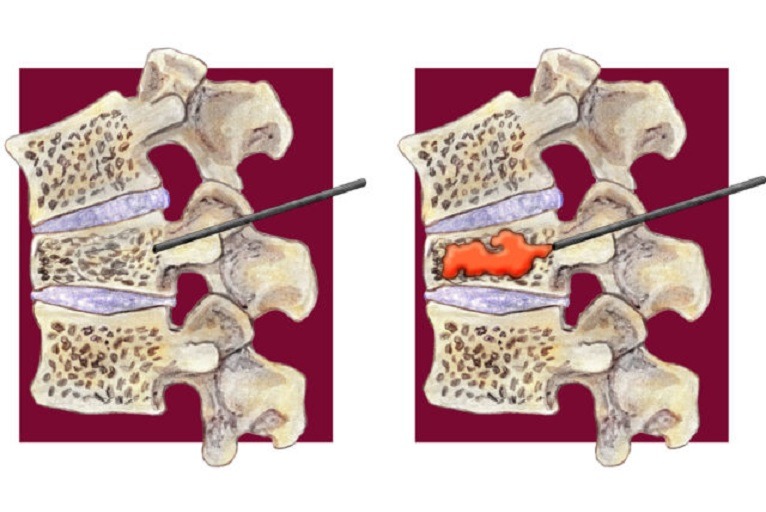
Minimally invasive spine surgery may involve percutaneous (through the skin) or mini-open (small incision) procedures. Instead of cutting through soft tissues, segmental tubular retraction creates an expandable tunnel that passes between muscles to access the spinal column. An endoscope, a tiny video camera, projects visualization of the surgical area on a monitor during the procedure to the spine surgeon. The surgery is performed through the tubular retraction system utilizing specially designed instruments.
Types of surgical procedures performed minimally invasively include Discectomy or Microdiscectomy, Foraminotomy or Microforaminotomy, Micro laminectomy and Microlaminotomy.
Surgical imaging systems and image-guidance Technologies, such as fluoroscopy (real-time x-ray), are utilized during surgery to pinpoint key aspects of the patient’s spinal anatomy. Furthermore, surgical imaging projects 2D and 3D views and guides placement of instrumentation, such as pedicle screws.
4 Spinal Disorders Treated Using MISS
Degenerative disc disease
Degenerative disc disease (DDD) usually develops gradually in older adults affecting the spine’s intervertebral discs. Normal cellular age-related changes in the body can cause discs to stiffen, lose flexibility, strength, height and shape, and the ability to absorb and distribute forces associated with movement. These structural changes may increase the risk of disc herniation.
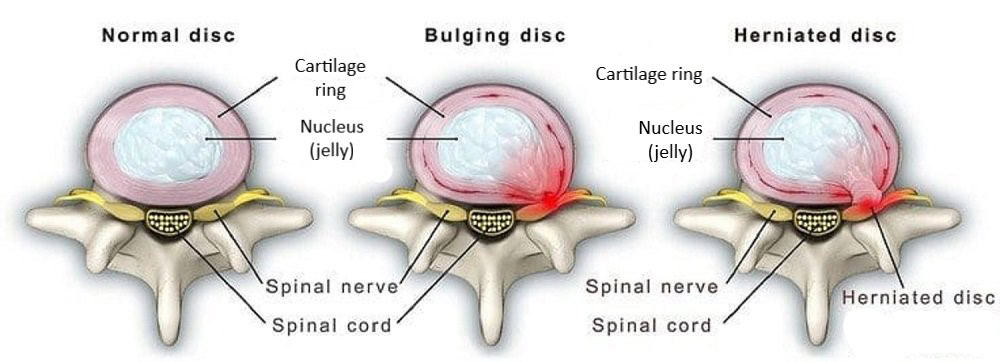
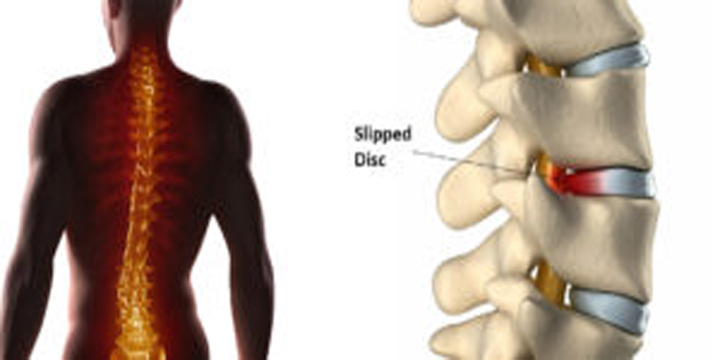
Herniated discs
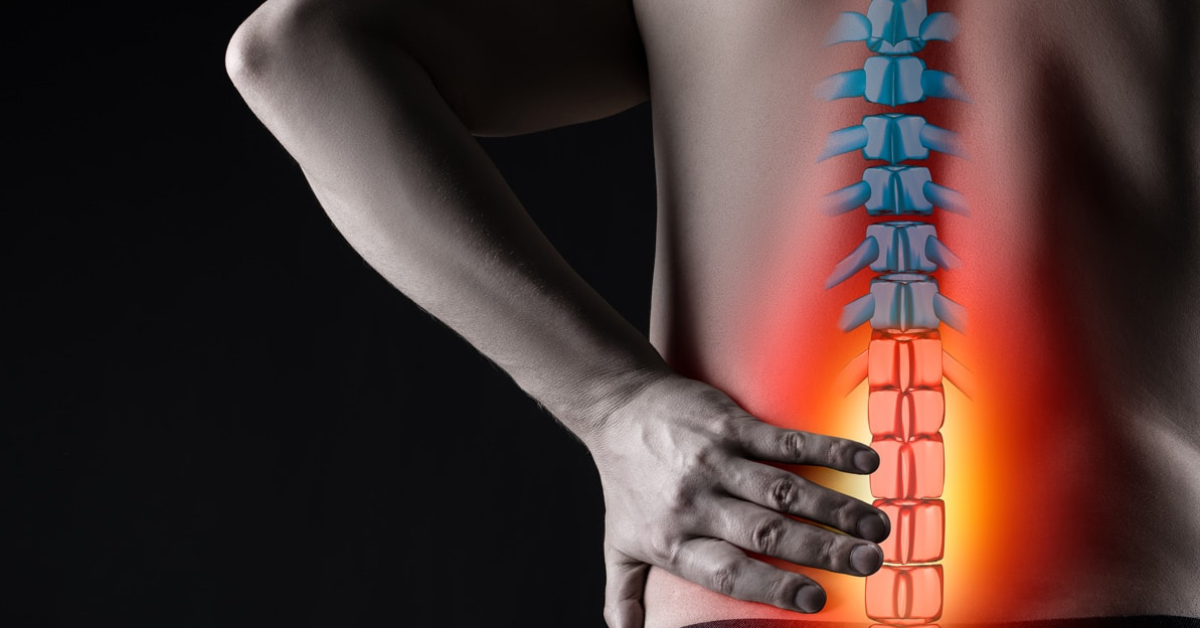
A herniated disc sometimes called a slipped disc or ruptured disc occurs when the gel-like inner core of an intervertebral disc breaks through the protective outer layer of the disc. Besides the damaged disc, the interior gel can irritate and inflame nearby spinal nerves and cause back pain.
Scoliosis
Scoliosis is an abnormal sideward curve of the spine that may cause progressive spinal deformity. A scoliotic curve may resemble an “S” or “C.” Most cases of scoliosis have no known cause—and while the condition is mostly associated with children, adults can develop scoliosis, too.
Spinal stenosis
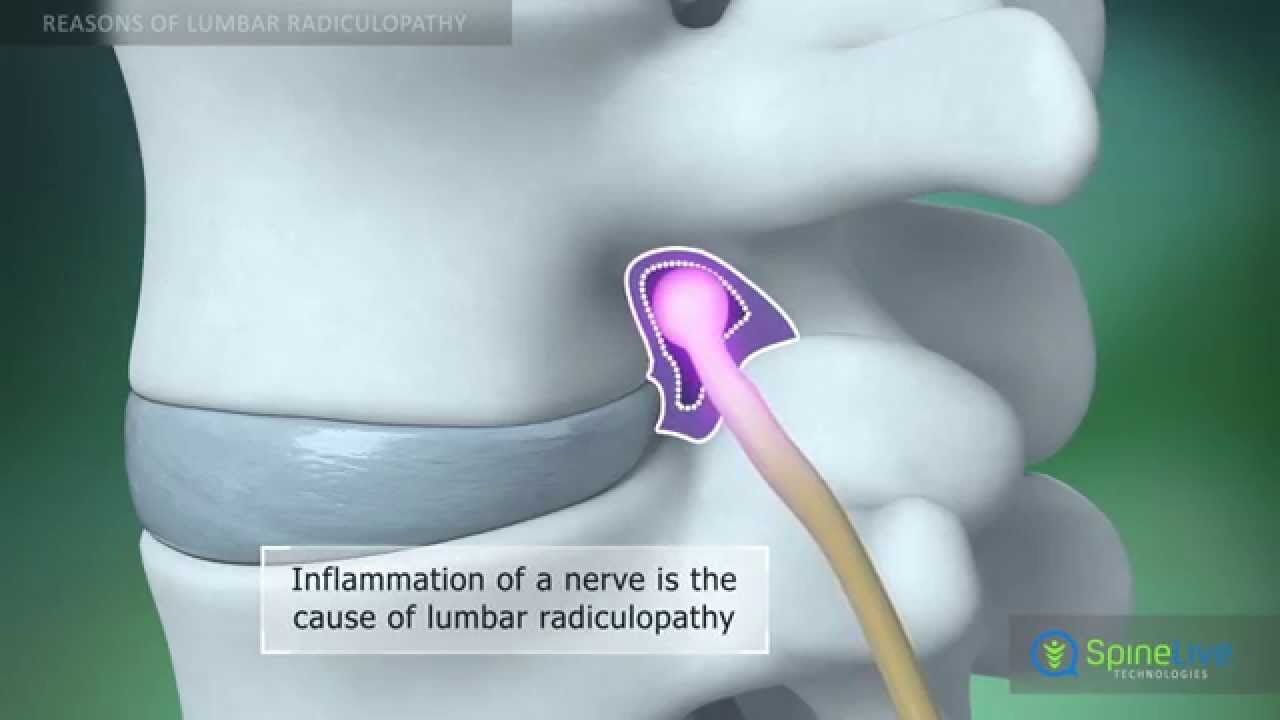
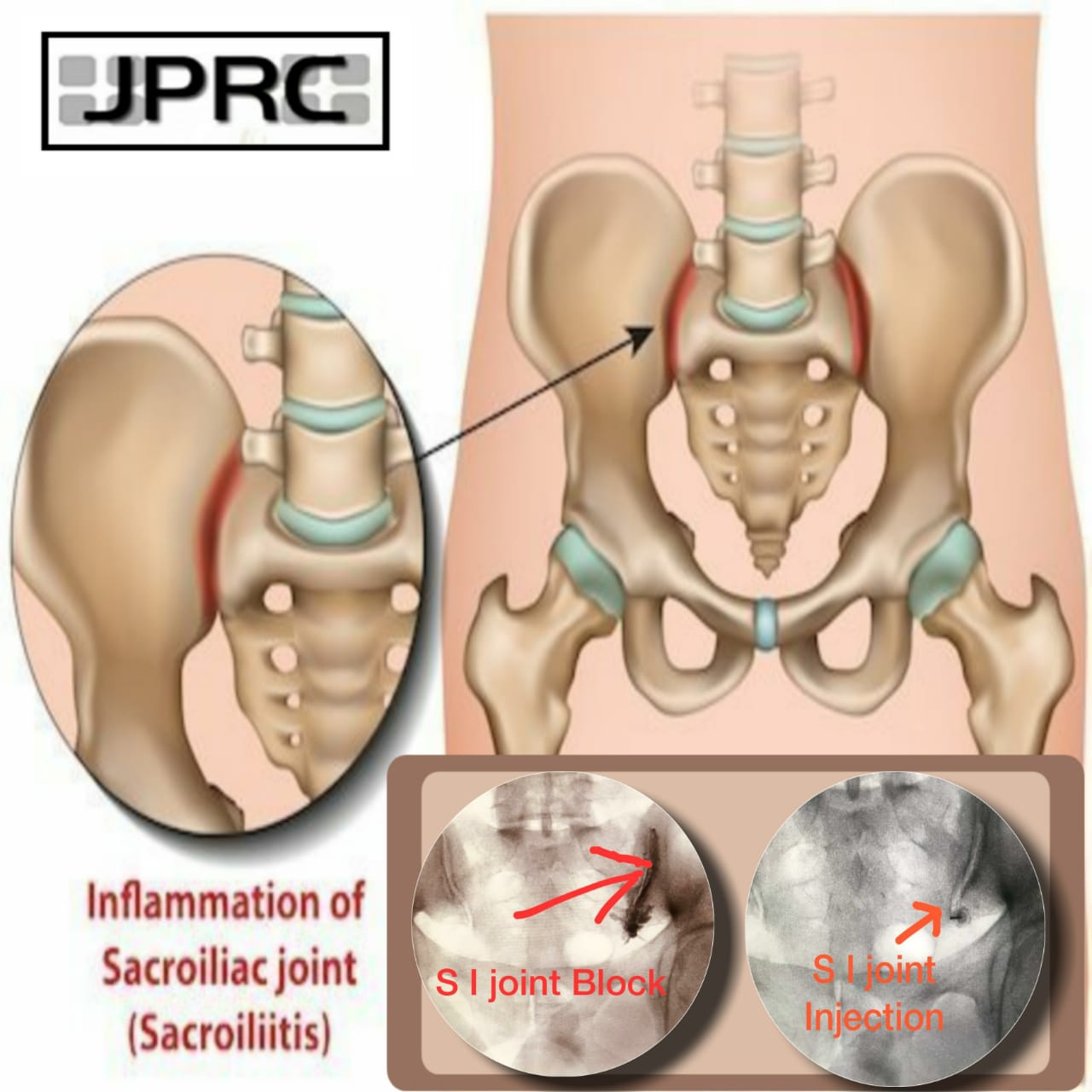
Spinal stenosis occurs when spinal nerve roots and/or the spinal cord become compressed. The nerve roots branch off the spinal cord and exit the spinal canal through passageways called neuroforamen. Nerve and/or spinal cord compression can cause symptoms such as pain, weakness, tingling sensations, and numbness. Sometimes, pain and symptoms travel into the arms or legs.
Risks of Minimally Invasive Spine Surgery
Any type of spine surgery offers potential benefits and risks—complications can occur. Listed below are several possible complications that may occur during and/or after spine surgery—both open and minimally invasive spine surgical procedures.
- Bleeding
- Blood clots
- Nerve damage
- Return of symptoms
- Failed fusion (known as pseudarthrosis or non-union)
- Infection
Are You a Candidate for Minimally Invasive Spine Surgery?
Minimally invasive spine surgery offers many benefits:
* Smaller incisions
* Less pain
* Fewer risks
* Quicker recovery times.
However, MISS is still a surgical procedure. Keep in mind that less than 5% of people with back or neck pain need spine surgery— and, surgery should be the last resort for treating pain caused by a spinal disorder.
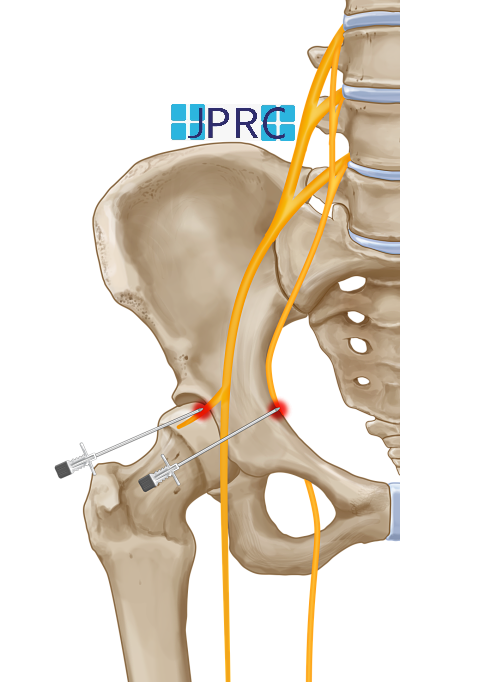
If non-surgical treatments, such as medications, physical therapy, and/or spinal injections do not effectively reduce symptoms in 3 to 6 months, then you may be a candidate for Spine surgery. Of course, certain types of spinal disorders warrant urgent or immediate Surgical intervention. Talk openly with your doctor or spine specialist about your pain and symptoms, along with the results of different therapies you’ve tried. There are many considerations you and your doctor need to discuss before making a surgical decision to treat back or neck pain—and if Minimally Invasive Spine Surgery may be an option for you.




















































.jpg)










_Injection_Description_in_Hindi.jpg)














.jpg)









.jpg)




.jpg)
.jpg)
.jpg)






.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)








1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)









2.jpg)
3.jpg)



4.jpg)
1.jpg)
2.jpg)

5.jpg)
6.jpg)


7.jpg)
2.jpg)

8.jpg)

9.jpg)
3.jpg)

10.jpg)

11.jpg)


12.jpg)
4.jpg)