cervical spondylosis
What Is Cervical Spondylosis?
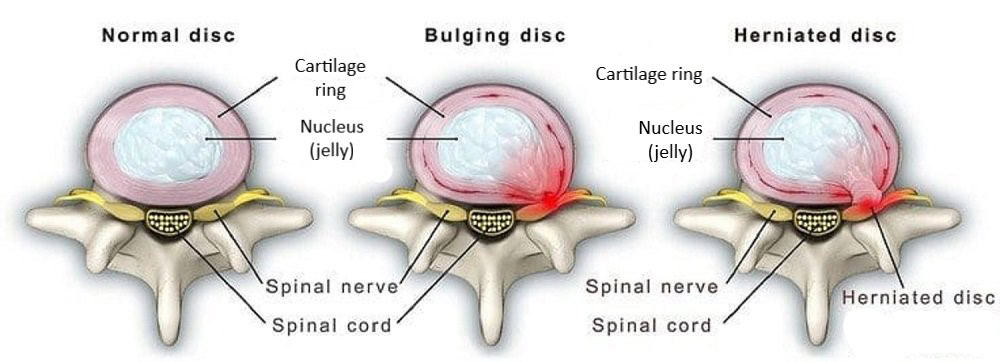
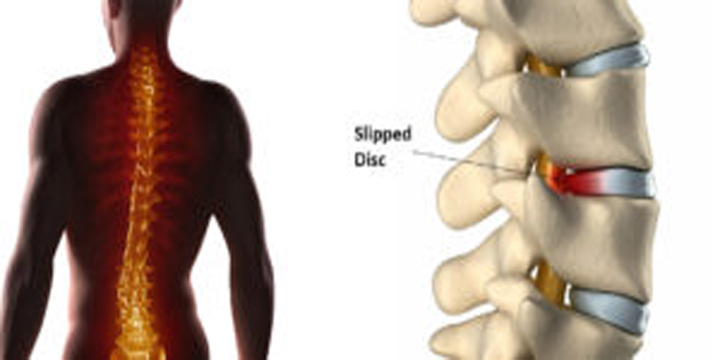
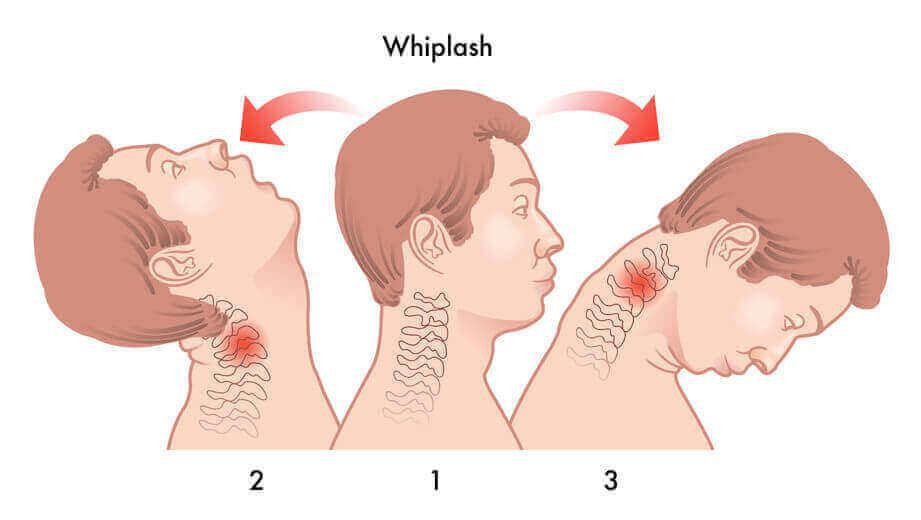
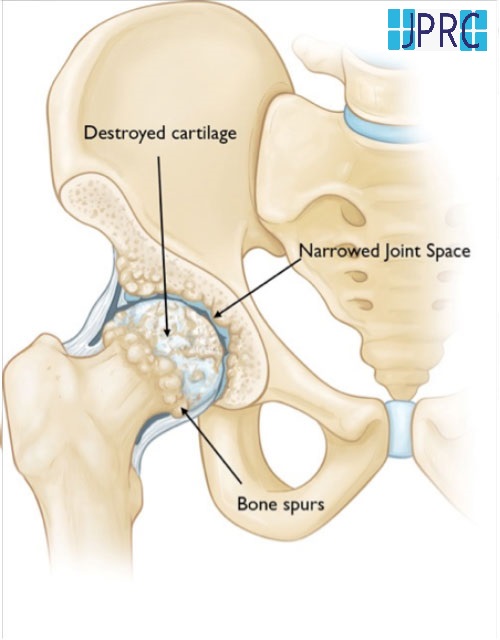
Cervical spondylosis is also called Cervical Osteoarthritis. It is a condition involving changes to the bones, discs, ligaments and facet joints of the neck. These changes are caused by the normal wear-and-tear of ageing. With age, the discs of the cervical spine gradually break down, facet joint degeneration, lose fluid, and become stiffer. Cervical spondylosis usually occurs in middle-aged and elderly people.
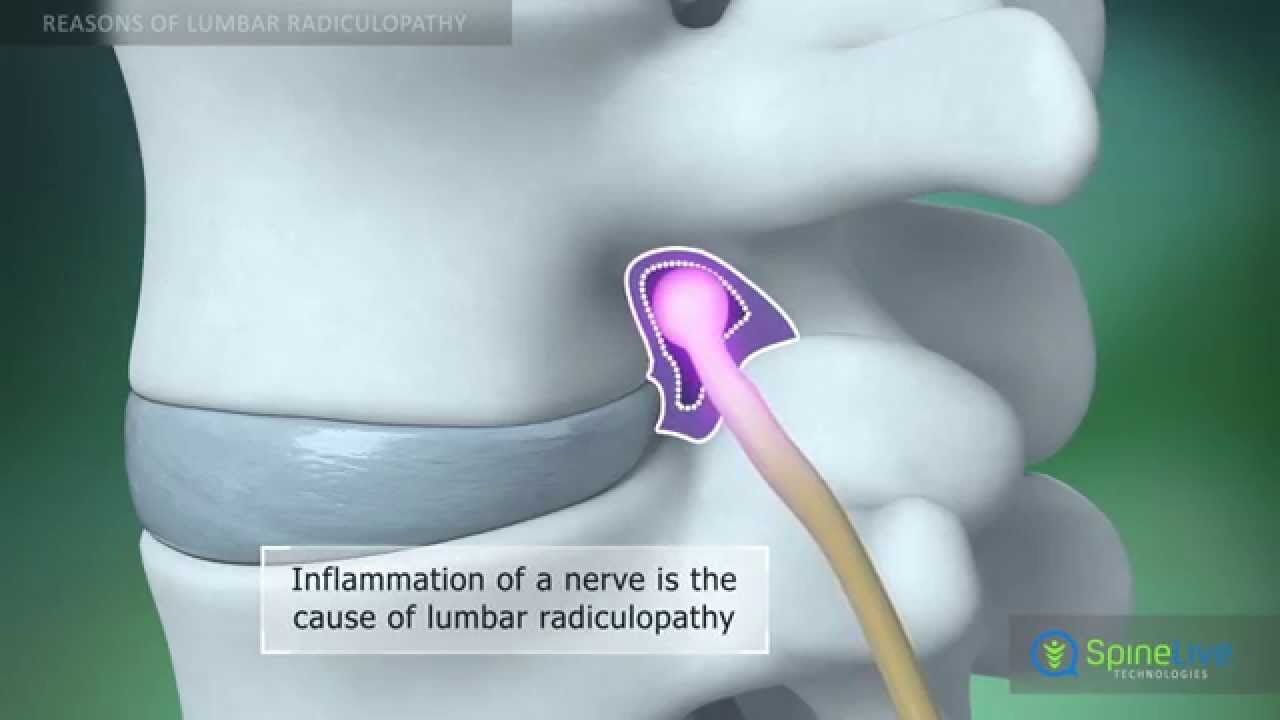
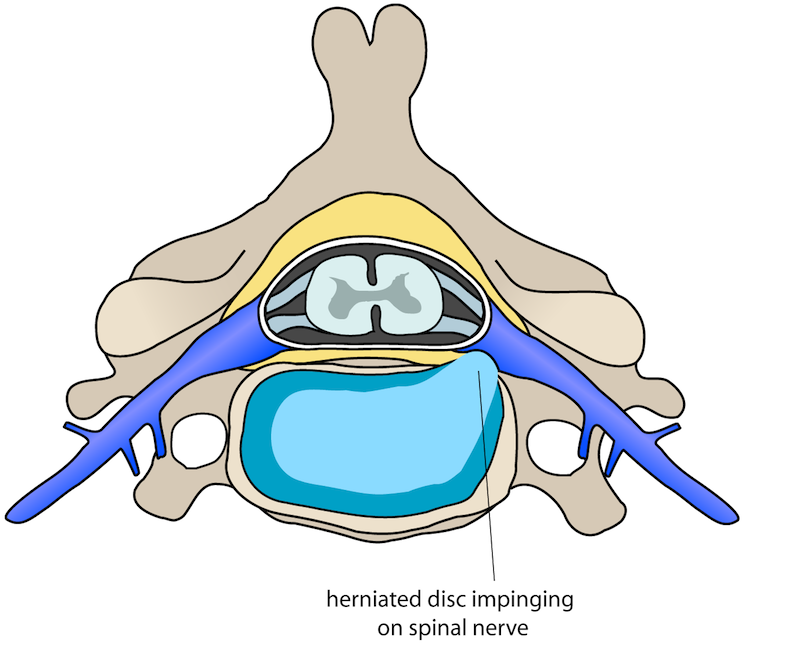
As a result of the degeneration of discs and other cartilage, spurs or abnormal growths called osteophytes may form on the bones in the neck. These abnormal growths can cause narrowing of the interior of the spinal column or in the openings where spinal nerves exit, a related condition called cervical Spinal Stenosis.
Cervical spondylosis most often causes Neck Pain and stiffness. Although cervical spondylosis is rarely progressive, corrective surgery can be helpful in severe cases.
What Are the Symptoms of Cervical Spondylosis?
The symptoms of cervical spondylosis include:
- Neck stiffness and pain
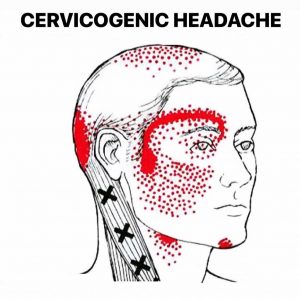
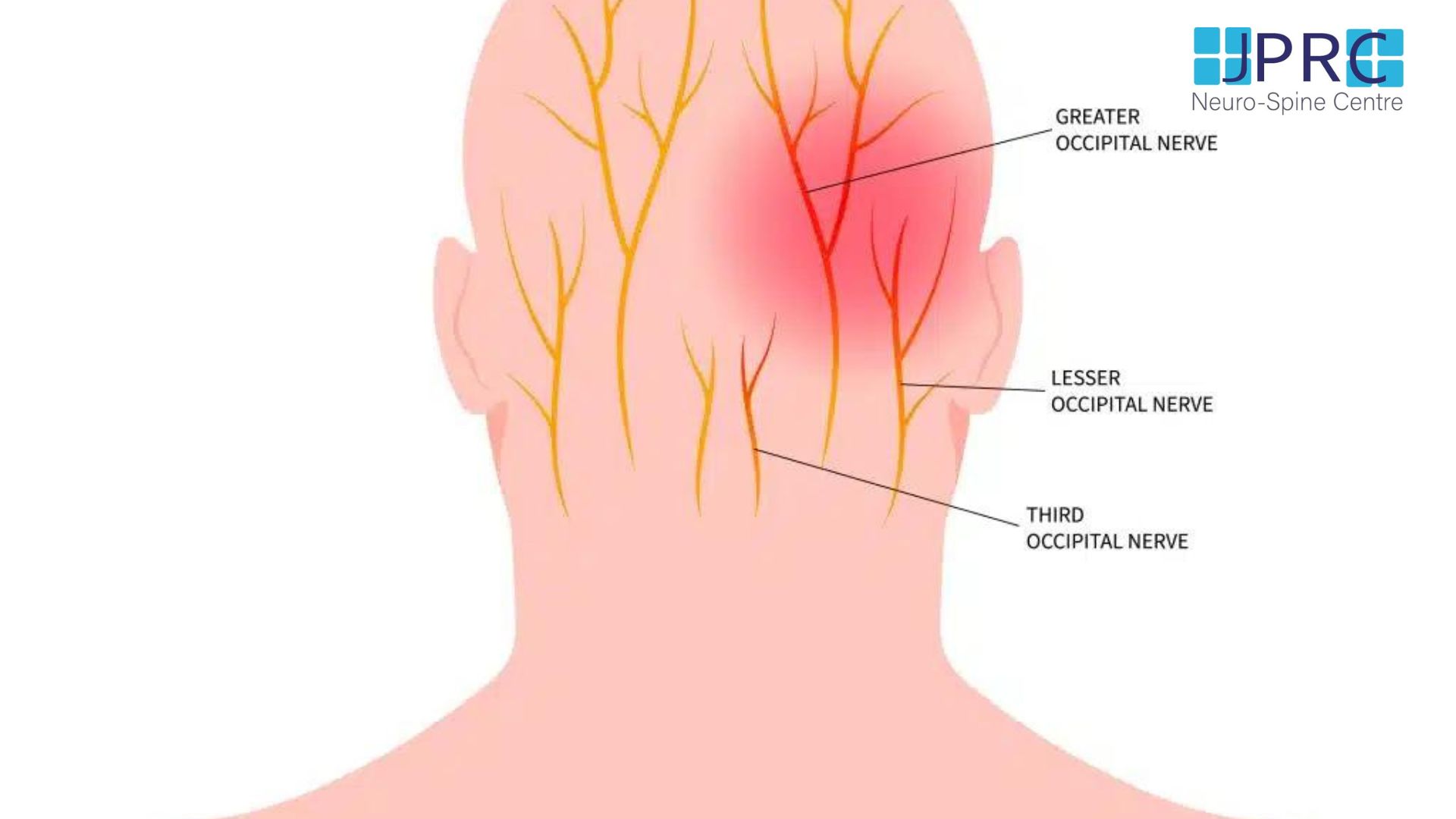
- Localised headache that may originate in the neck
- Pain in one or both shoulders or arms
- Inability to fully turn the head or bend the neck, sometimes interfering with driving
- Grinding noise or sensation when the neck is turned, sounding neck.
Symptoms of cervical spondylosis tend to improve with rest. Symptoms are most severe in the morning and again at the end of the day.
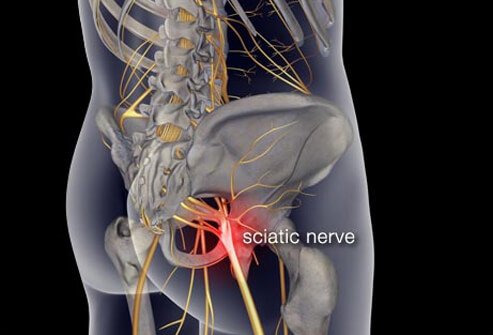
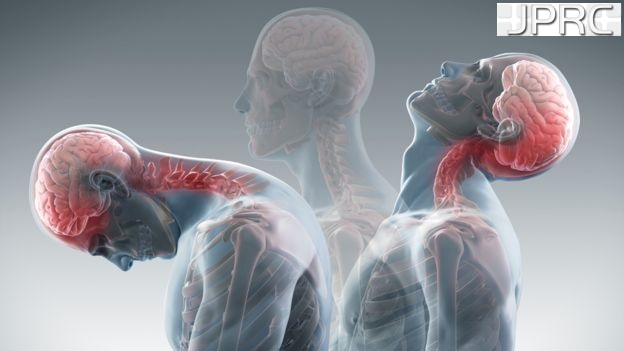
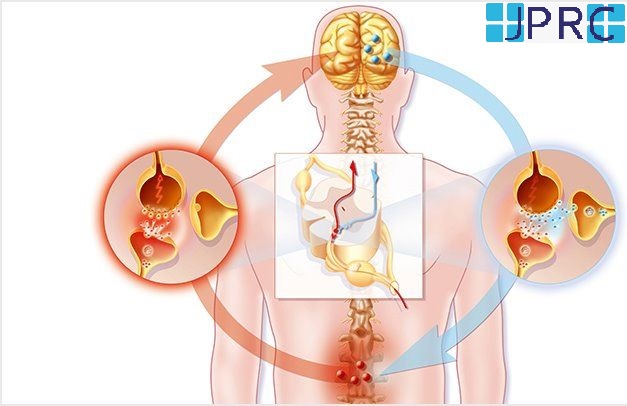
If cervical spondylosis results in pressure on the spinal cord (cervical stenosis), it can put pressure on the spinal cord, a condition called cervical myelopathy. Symptoms of cervical spondylosis with myelopathy include:
- Tingling, numbness, and/or gradual weakness in the arms, hands, legs, or feet
- Lack of coordination and difficulty walking
- Abnormal reflexes
- Muscle tightness or spasm
- Loss of control over bowel and bladder lead to incontinence.
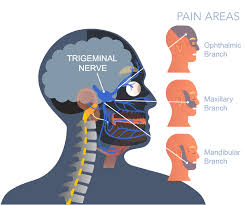
Another possible complication of cervical spondylosis is cervical myelopathy when bony spurs press on nerves as they exit the bones of the spinal column. Pain shooting down into one or both arms is the most common symptom.
How Is Cervical Spondylosis Diagnosed?
The doctor will generally begin by asking you about symptoms and taking a medical history. This will be followed by a clinical examination of the body, with a focus on the neck, back, and shoulders. The doctor is also likely to test reflexes and the strength of hands and arms, check for loss of sensation and watch you walk.
Other tests that might be done include imaging exams such as X-rays, computed tomography (CT), and (MRI). MRI scans use large magnets, radio waves, and a computer to produce the best images of the body. You might also be referred to a pain physician, neurosurgeon or neurologist.
What Are the Treatments for Cervical Spondylosis?
- Conservative treatment
- Rest
- Use of nonsteroidal anti-inflammatory drugs or other non-narcotic products to relieve pain from inflammation
- Wearing a cervical collar to limit movement and provide support
- Other forms of therapy including the application of heat and cold therapy, traction, or Exercises
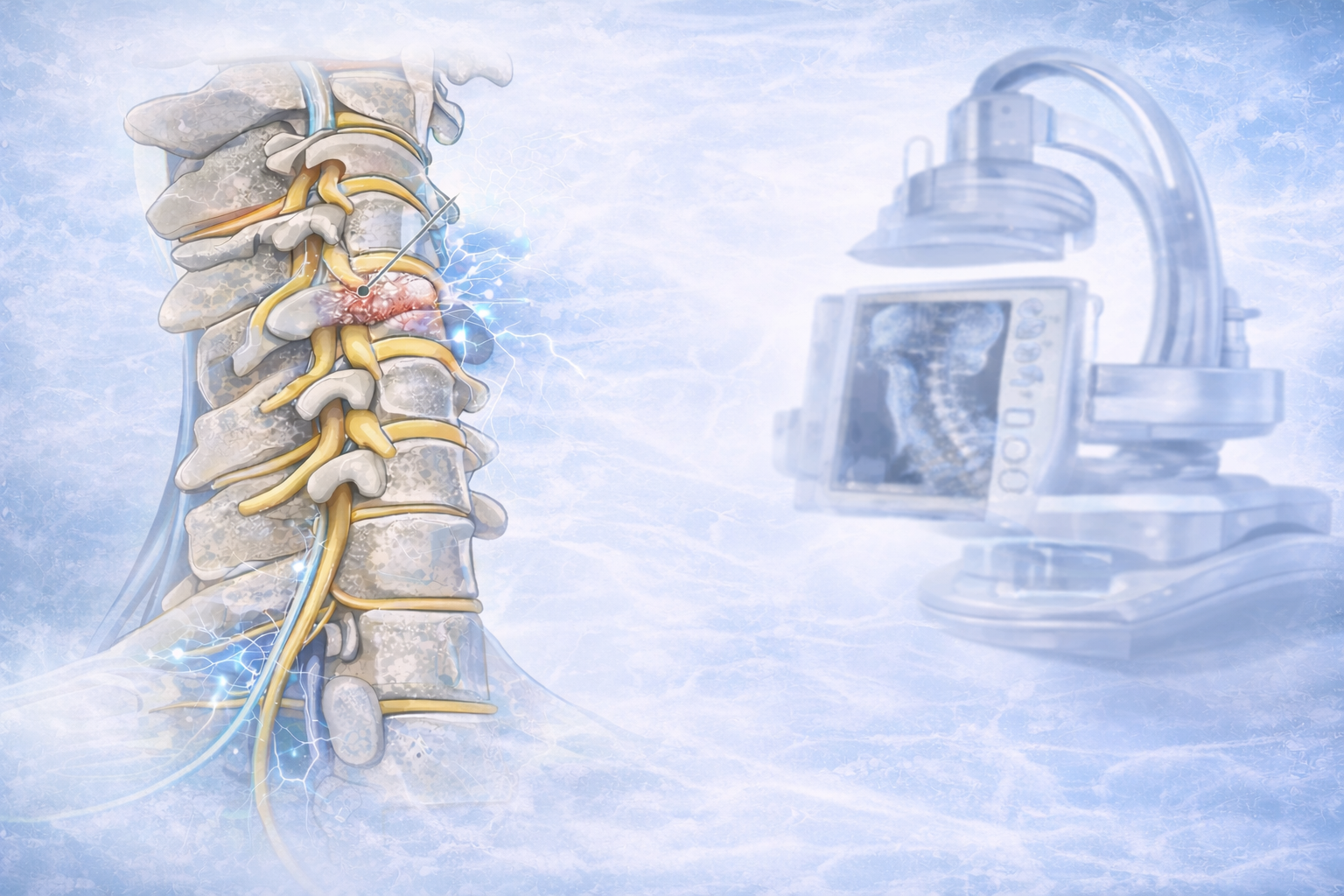
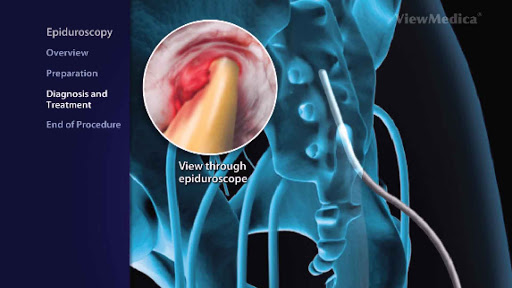
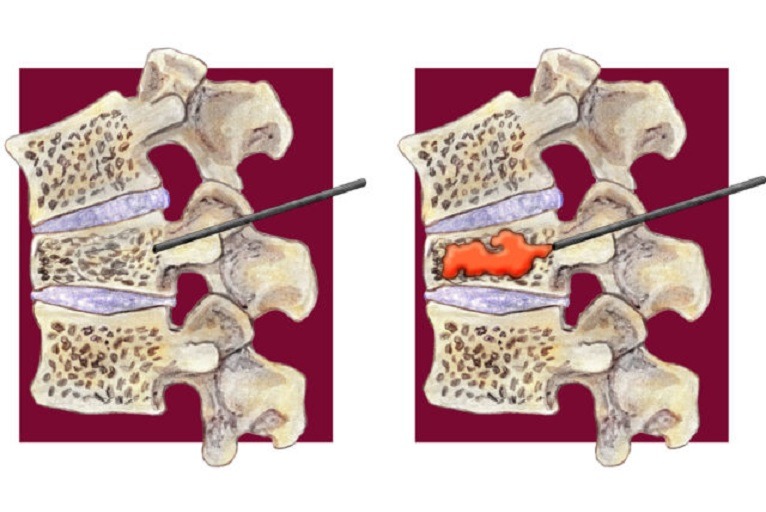
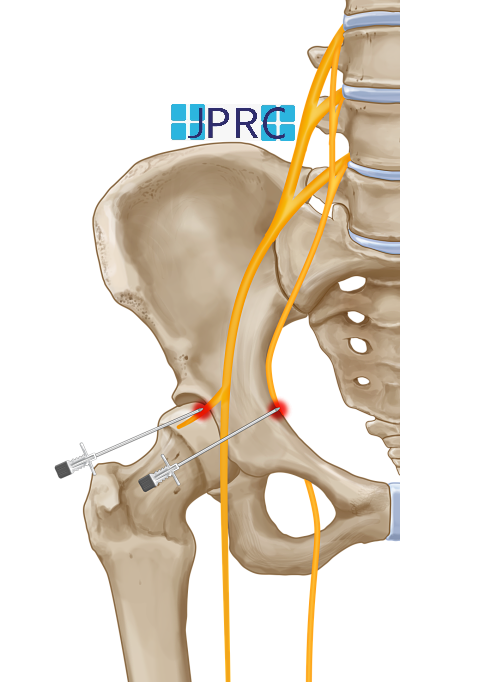
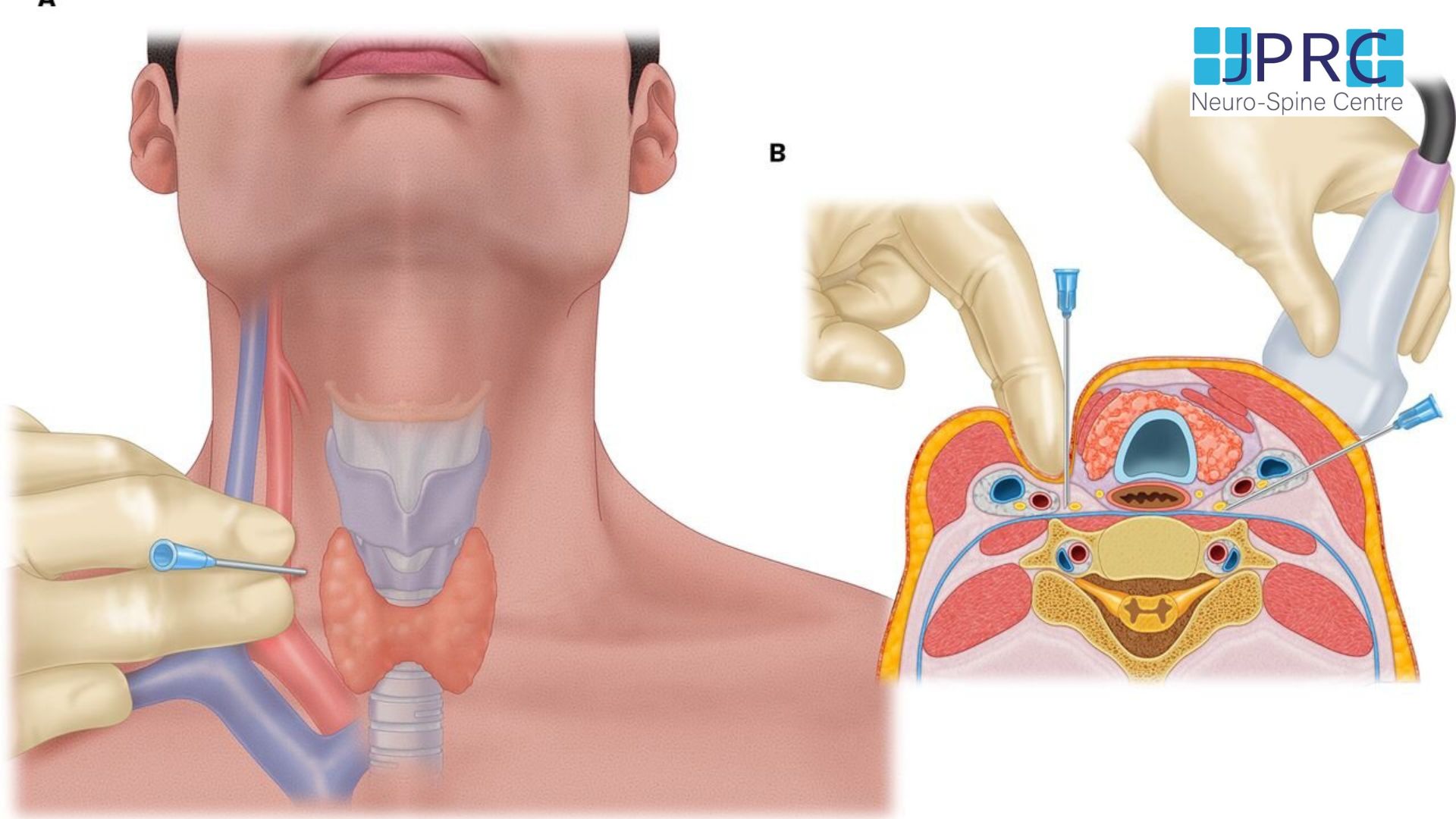
- Injecting drugs (corticosteroids and a local anaesthetic) into the joints of the cervical spine or the area surrounding the cervical spine known as Epidural injection or cervical facet joint injection
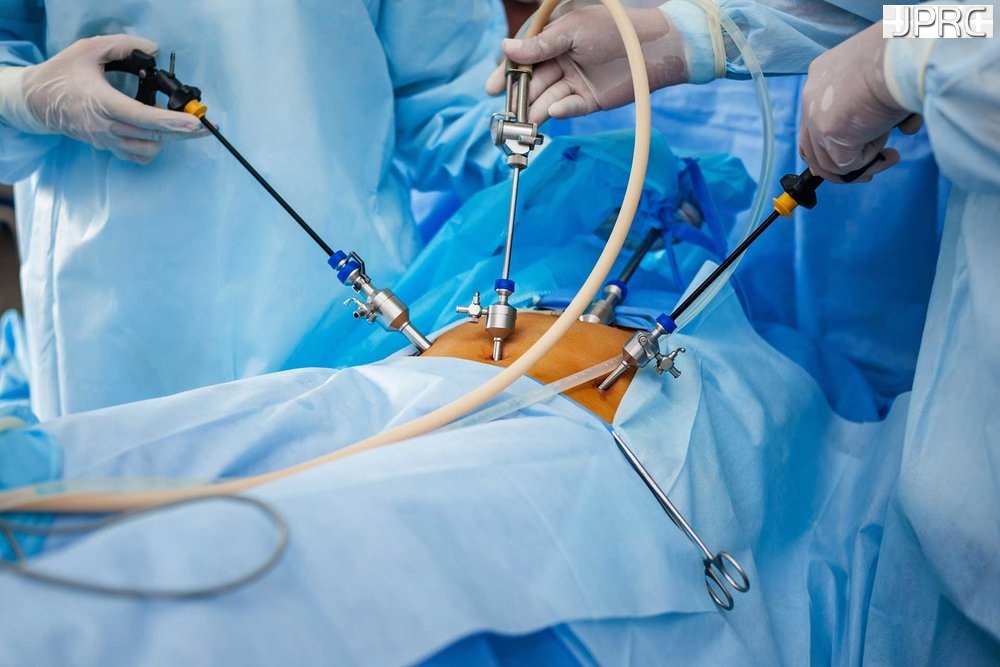
When Is Surgery Needed for Cervical Spondylosis?
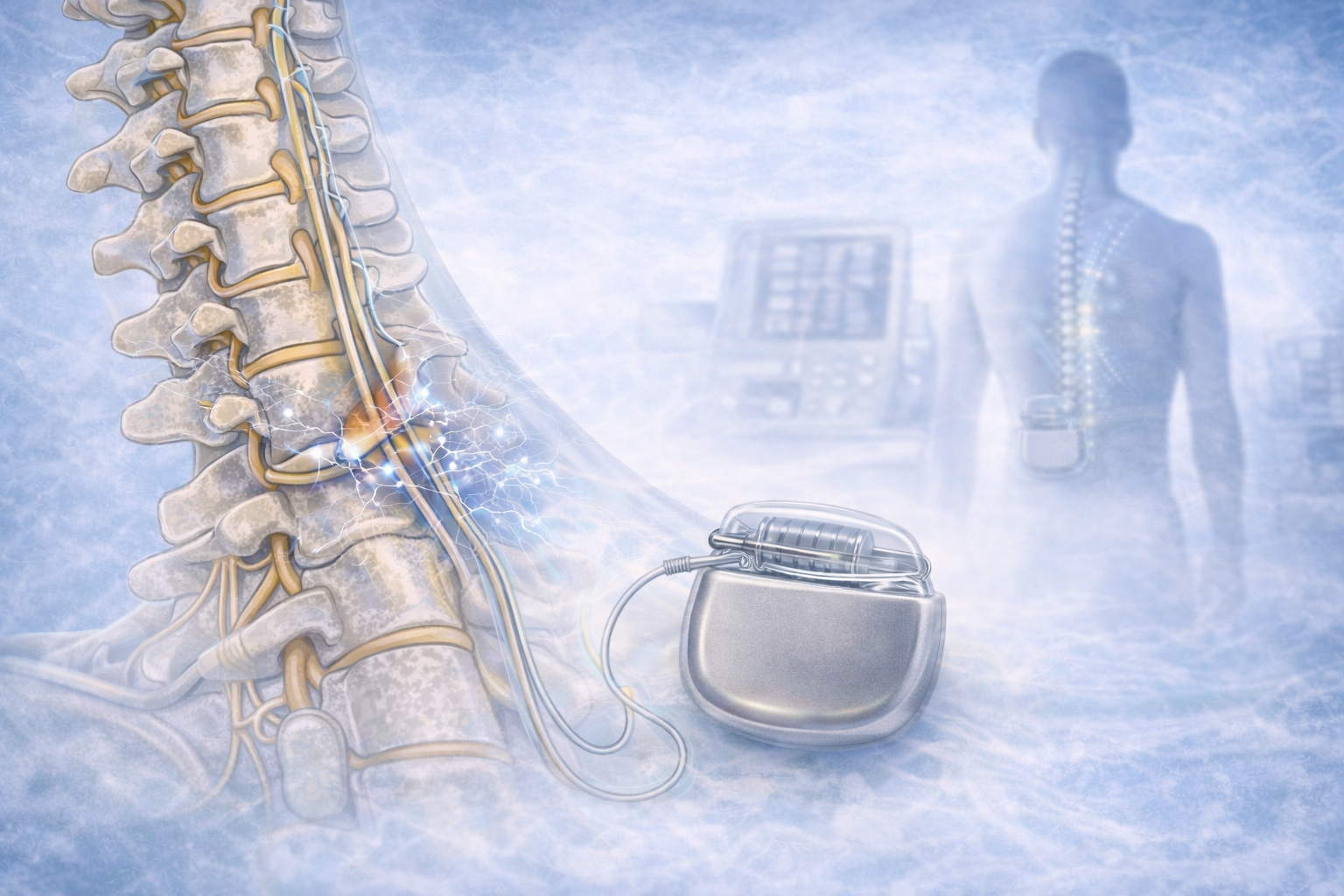
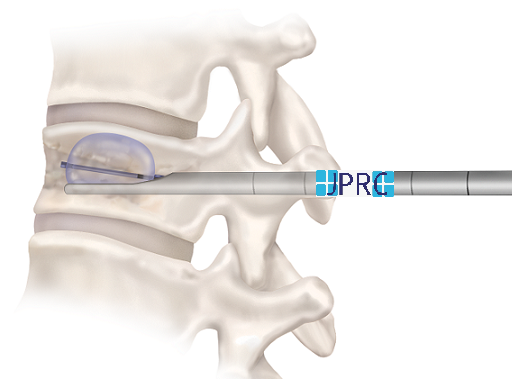
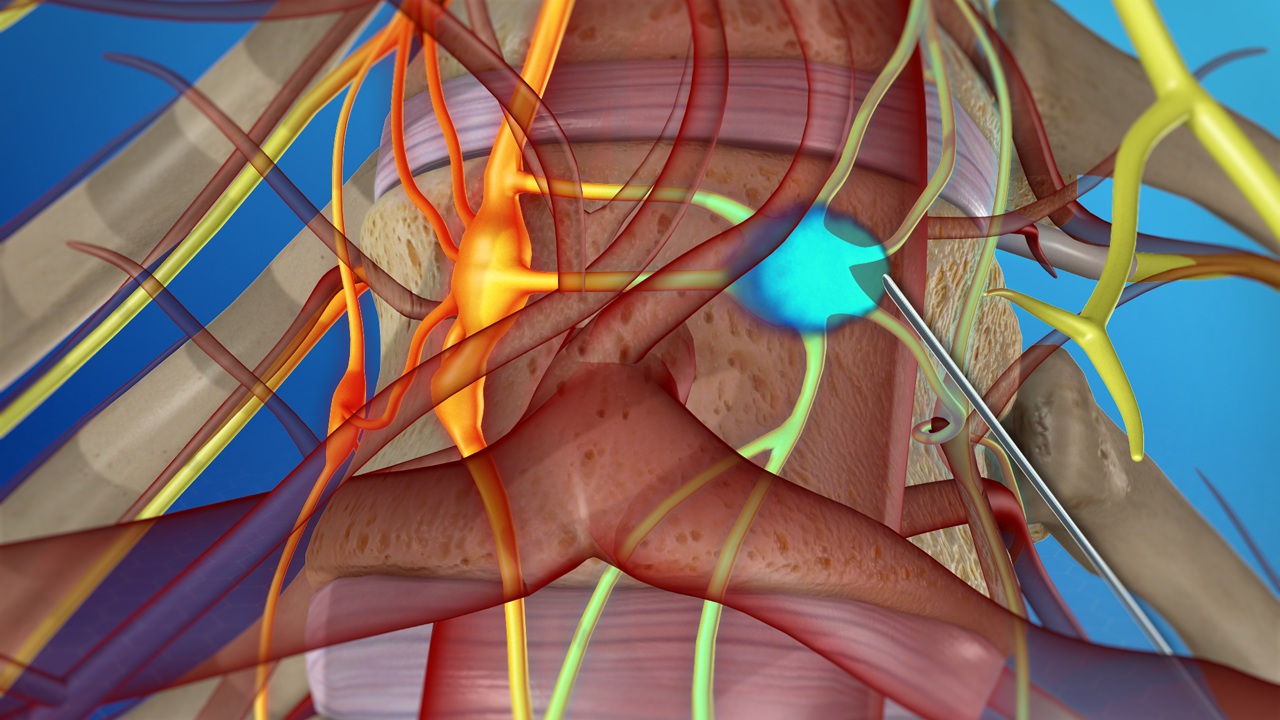
Cervical spondylosis tends to be a chronic (long-term) condition. But in most cases, it is not progressive. Surgery is required only in rare cases. The goal of surgery is to remove the source of pressure on the spinal cord and nerves. The surgery may also include adding stabilization in the form of implants or through the fusion of the vertebrae. But surgery is considered only when there is a severe loss of function. For instance, it might be considered if you had a progressive loss of feeling and function in your arms, legs, feet, or fingers. Any type of spinal cord compression could result in permanent functional disability.
The neurosurgeon can approach the cervical spine from the front (anterior) or the back (posterior). Approaching from the front might be used to remove the discs and spurs that are causing pressure. The disc may be replaced with an implant. A more extensive surgery calls for the removal of both discs and parts of the vertebra. These parts are replaced with a bone graft or implant.




















































.jpg)










_Injection_Description_in_Hindi.jpg)














.jpg)









.jpg)




.jpg)
.jpg)
.jpg)






.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)








1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)









2.jpg)
3.jpg)



4.jpg)
1.jpg)
2.jpg)

5.jpg)
6.jpg)


7.jpg)
2.jpg)

8.jpg)

9.jpg)
3.jpg)

10.jpg)

11.jpg)


12.jpg)
4.jpg)