BackPain sometime maybe metastatic cancer?
Metastatic Disease
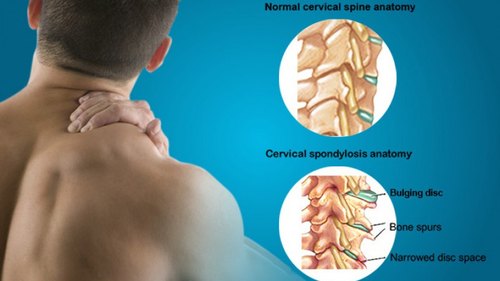
The spine accounts for 80% of bone metastatic lesions and is one of the most common sites for the early presentation of metastases. Cancer of the breast, lung, and prostate are the most commonly associated with bony metastases and up to 50% of patients with these types of cancer will develop bone metastases, Approximately 60% of bone metastases are found in the axial skeleton. Studies have shown that the majority of skeletal metastases can be asymptomatic with cervical and lumbar metastases tending to be more symptomatic than those in the thoracic spine. Unfortunately, metastatic disease is typically wide-spread by the time patients present symptomatically to the clinic.
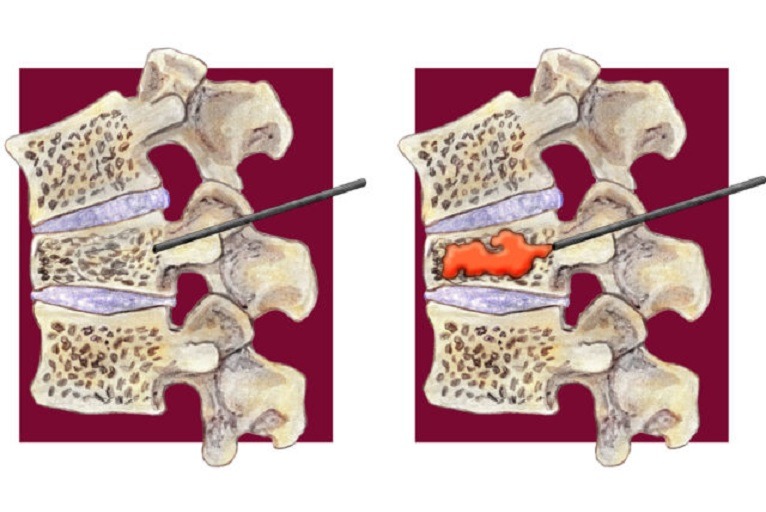
Once symptoms present, delays in diagnosis can be significant. Studies have shown symptom-to-diagnosis delay in lung cancer to be approximately 1–3 months. Overall diagnostic delay is mostly attributed to patient delay in seeking proper care. Delays related to the practitioner tend to be of shorter duration. Misdiagnosis and misinterpretation of tests are two factors contributing to practitioner delay. The inherently poor sensitivity of radiographs in detecting metastatic lesions can lead to misdiagnosis, adding to practitioner delay. More specifically, bony destruction of 30–50% is necessary for a lytic lesion to appear on radiographs, suggesting that some metastatic lesions may go undetected by radiographs for a considerable period of time for a couple of months total Diagnostic delay was approximately 128 days with 92 days attributed to practitioner delay. Notably, the patient had received conventional radiographs of the lumbar spine at initial presentation to the Treating physician or physiotherapist, which showed no signs of metastatic disease.
Most non-musculoskeletal causes of back pain do not specifically target the upper lumbar spine. hematogenous seeding (i.e. osteomyelitis or metastatic carcinoma) can be spread throughout the body with areas near the venous/lymphatic drainage being the most highly affected. In the case of lung cancer, the thoracic spine is the most common region for spinal metastases
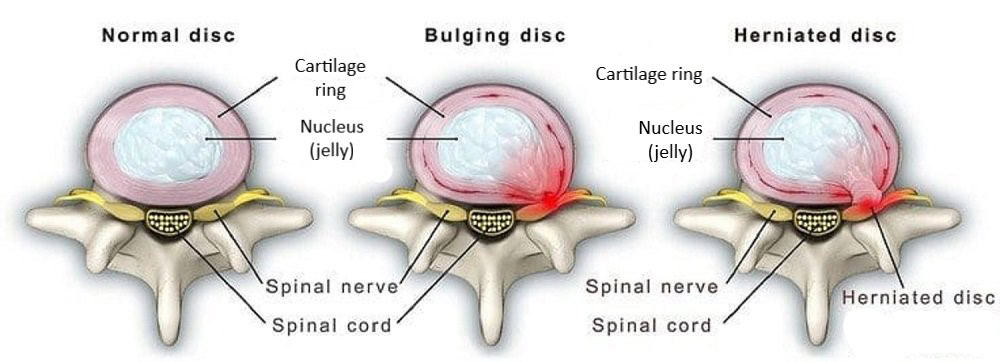
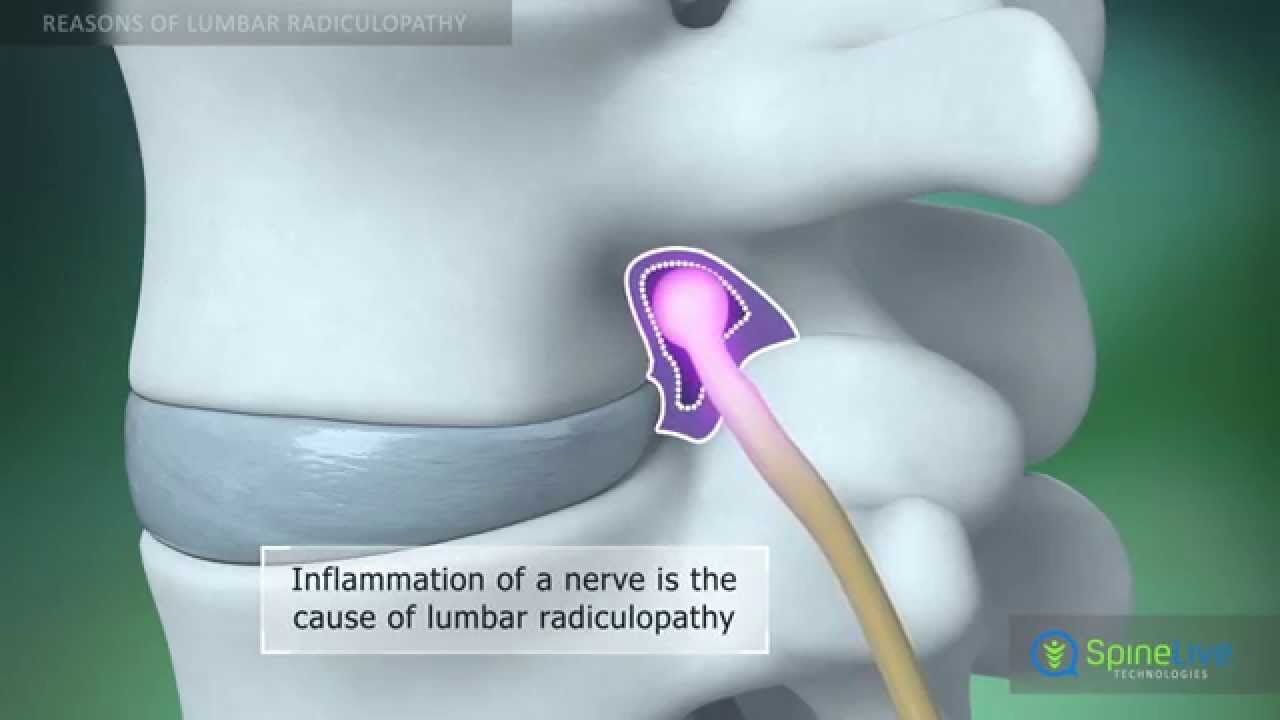
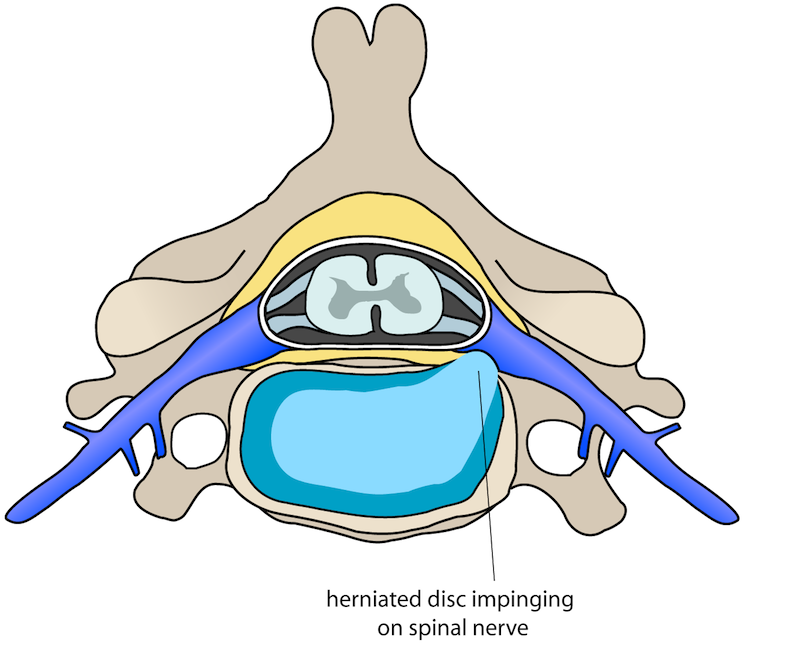
The upper lumbar spine only accounts for 2–4% of lumbar disc herniations, 8% of lumbar facet arthropathies,35% of lumbar central canal stenosis, and 9–11% of lumbar degenerative disc disease (DDD). Degenerative disc disease isolated to the upper lumbar spine is even rarer, accounting for only 2% of lumbar DDD patients.
How a patient has gone through spinal pain in cancer[metastasis].
The patient was a 48-year old working woman (height = 165 cm; mass = 92.7 kg). She occasional walking for physical activity. The patient smoked 05 cigarettes per day for the last 15 years She also had a history of anxiety and major depression, both of which were managed by a psychiatrist and were currently under control.
She was originally evaluated in the emergency orthopaedic department the day after the onset of low back pain symptoms. Lumbar radiographs were significant for degenerative changes at the L5-S1 level. A urinalysis was unremarkable. She was diagnosed with a lumbar strain, prescribed naproxen, and asked to follow-up with her primary care physician if she did not improve.
There was no improvement 1 month after symptom onset when the patient was evaluated by her primary care physician. During this evaluation, the patient complained that her daily activities were being limited by fatigue. Of note, the patient had an 11-year clinical history of fatigue associated with her depression. She also noted that the pain was unchanged with activity. At this visit, she was prescribed diclofenac sodium, provided with a general exercise handout, instructed in postural education, advised on activity modification, instructed to rest and use heat, and referred to PT.
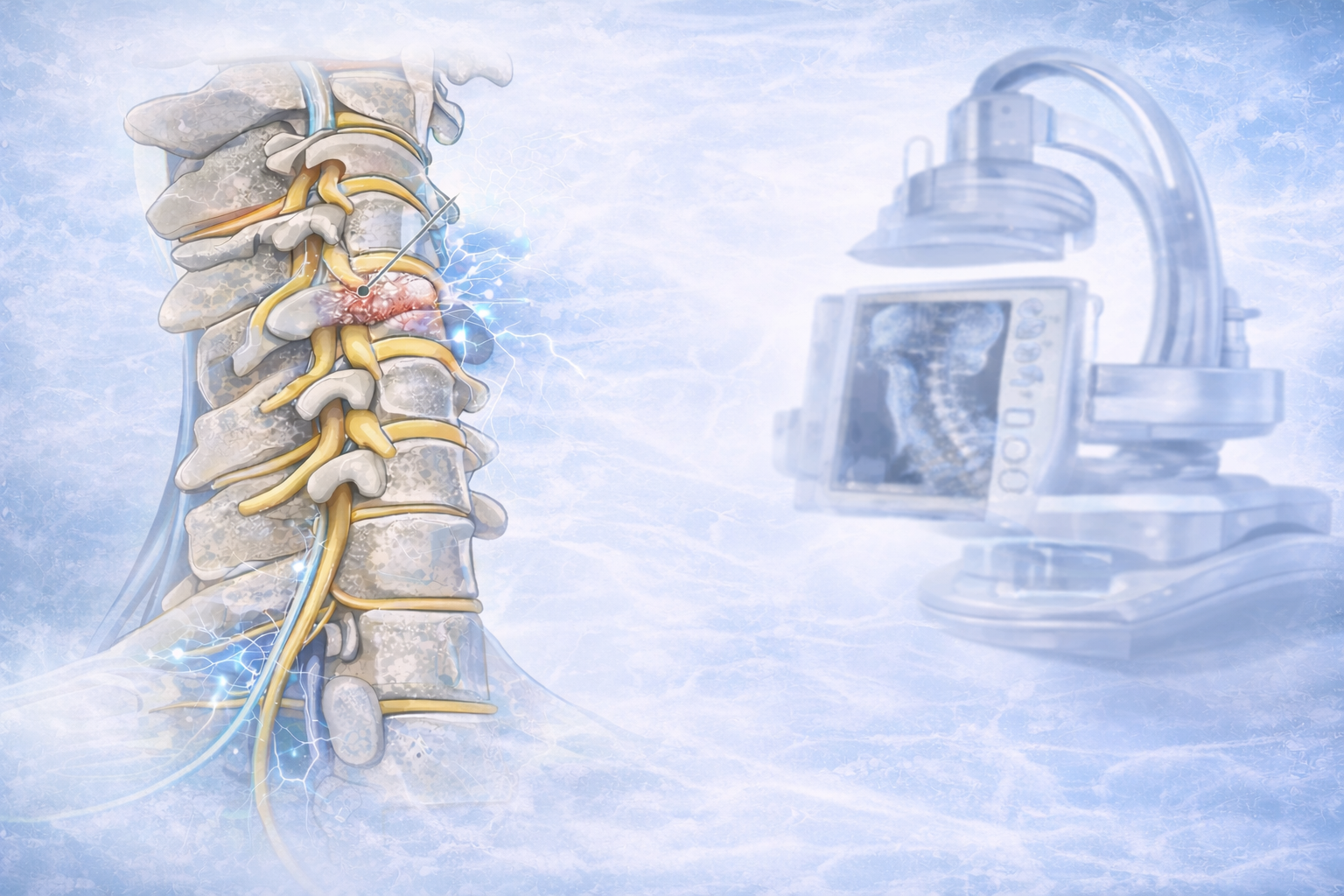
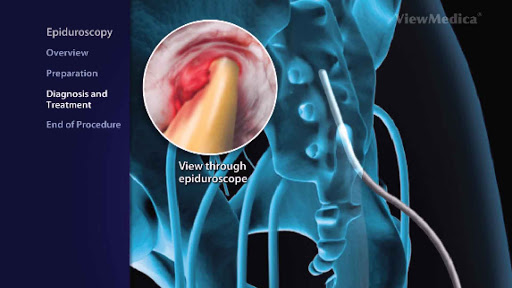
After a long trial patient, she decided to consult a pain physician who asks him to get done MRI whole spine and bones scan and pulmonary function test along with routine examination. after careful evaluation of all relevant investigation, now the situation was clear exactly. And the case was referred to an oncologist for further management.




















































.jpg)










_Injection_Description_in_Hindi.jpg)














.jpg)









.jpg)




.jpg)
.jpg)
.jpg)






.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)








1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)










2.jpg)
3.jpg)



4.jpg)
1.jpg)
2.jpg)

5.jpg)
6.jpg)


7.jpg)
2.jpg)

8.jpg)

9.jpg)
3.jpg)

10.jpg)

11.jpg)


12.jpg)
4.jpg)