Migraine and medical mangement
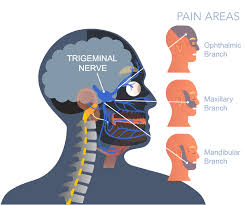
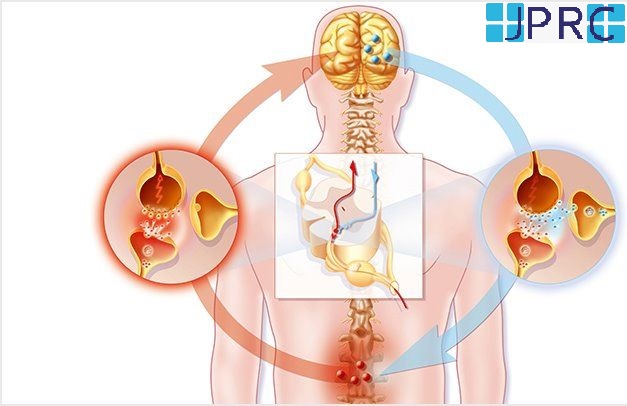
Migraine is a result of specific changes within the brain NEUROPHYSIOLOGY. It causes severe head pain that is often accompanied by sensitivity to light, sound, or smells.
-
Common symptoms include:
- Eye pain
- Hypersensitivity to light or sound
- Nausea
- Vomiting
- Severe pain, often only on one side of the head, that some individuals describe as "pounding" or throbbing
-
Types of migraines include:
- Common migraine has no "Aura.” About 80% of migraines are common.
- Classic migraines (migraine with aura) present with an aura before the headache and are more severe than common migraines.
- A silent or acephalgic migraine is a migraine without head pain but with aura and other aspects of migraine.
- Hemiplegic migraine can have symptoms that mimic a stroke, such as weakness on one side of the body, loss of sensation, or feeling "pins and needles."
- A Retinal migraine causes temporary vision loss in one eye, which can last from minutes to months, but it is usually reversible. This is often a sign of a more serious medical problem, and patients should seek medical care.
- Chronic migraine is a migraine headache that lasts for more than 15 days per month for three consecutive months.
- Status migrainosus is a constant migraine attack that lasts more than 72 hours.
Other types of headaches can also cause intense pain, and not all headaches are migraines. For example, some describe the pain of cluster headaches as the worst pain they have experienced. Sinus headaches can also cause pain and inflammation.
- The causes of migraines are not known may be idiopathic most often. Changes in neurotransmitter levels within the brain are thought to play a role.
- The presence of typical clinical signs and symptoms help diagnose migraines.
- Migraine attacks can be triggered by many factors, for example:
- Hormonal changes
- Stress induces
- Strong stimuli like loud noises
- Certain foods
Diet plays a vital role in preventing migraines. Many foods and beverages are known migraine triggers, such as:
- Foods with nitrates including hot dogs, deli meats, bacon, and sausage
- Chocolate
- Cheese that contains the naturally-occurring compound tyramine, such as blue, feta, cheddar, Parmesan, and Swiss
- Alcohol, especially red wine
- Foods that contain monosodium glutamate (MSG), a flavour enhancer
- Very cold foods such as ice cream or iced drinks
- Processed foods
- Pickled foods
- Beans
- Dried fruits
- Cultured dairy products such as buttermilk, sour cream, and yoghurt
A small amount of caffeine may ease migraine pain in some people. Caffeine is also in some migraine medications. But, too much caffeine may cause a migraine. It may also lead to a severe caffeine withdrawal headache.
-
Medical treatment
-
Pain relievers are typically the first drugs recommended by doctors for migraine and headaches. Many of these medications are over-the-counter, or available without a doctor's prescription, while other headache drugs require a prescription.
Note: if symptomatic relief medications are used more than twice a week, you should see your doctor, who may prescribe preventive headache medications. Overuse of symptomatic medications can actually cause more frequent headaches or worsen headache symptoms.
Medications for acute and chronic migraines
The treatment of an acute migraine headache may vary from over-the-counter (OTC) medicines, like acetaminophen ibuprofen, naproxen sodium medications.
Triptans
- Triptans (sumatriptan, rizatriptan, eletriptan, zolmitriptan, naratriptan, almotriptan, and frovatriptan), may be extremely effective in treating migraines and may be prescribed to help patients treat their migraines at home. A combination of naproxen and sumatriptan is now available. Additionally, sumatriptan is now available as a patch, which delivers the medication through the skin.
- Not every patient can take these medications, and there are specific limitations regarding how often these medications can be used.
- Other medication regimens may also be used to control migraine headache.
- Some medications are appropriate for home use and others require a visit to the doctor's office or emergency department.
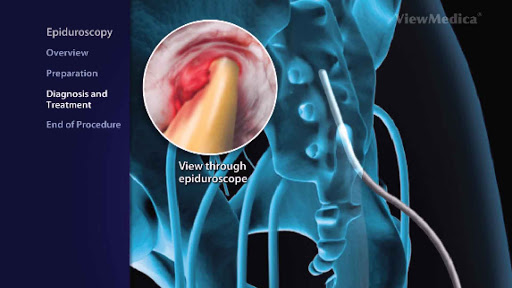
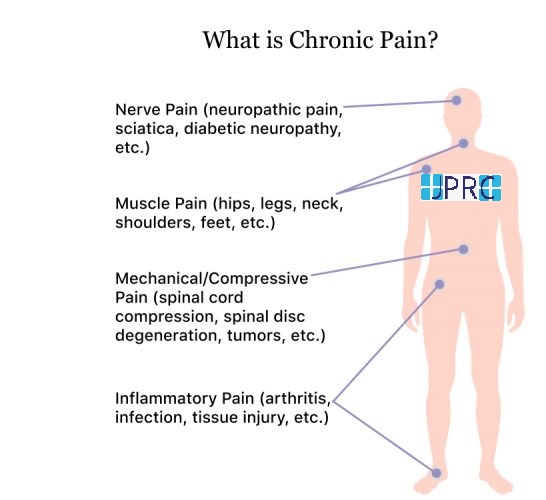
- Interventional pain management for migraine
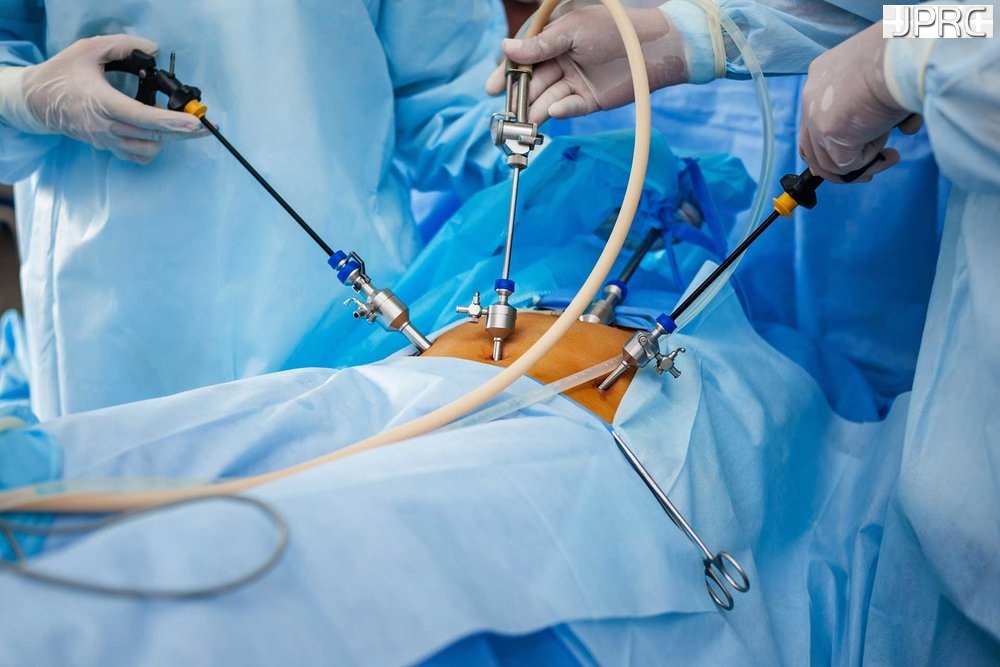
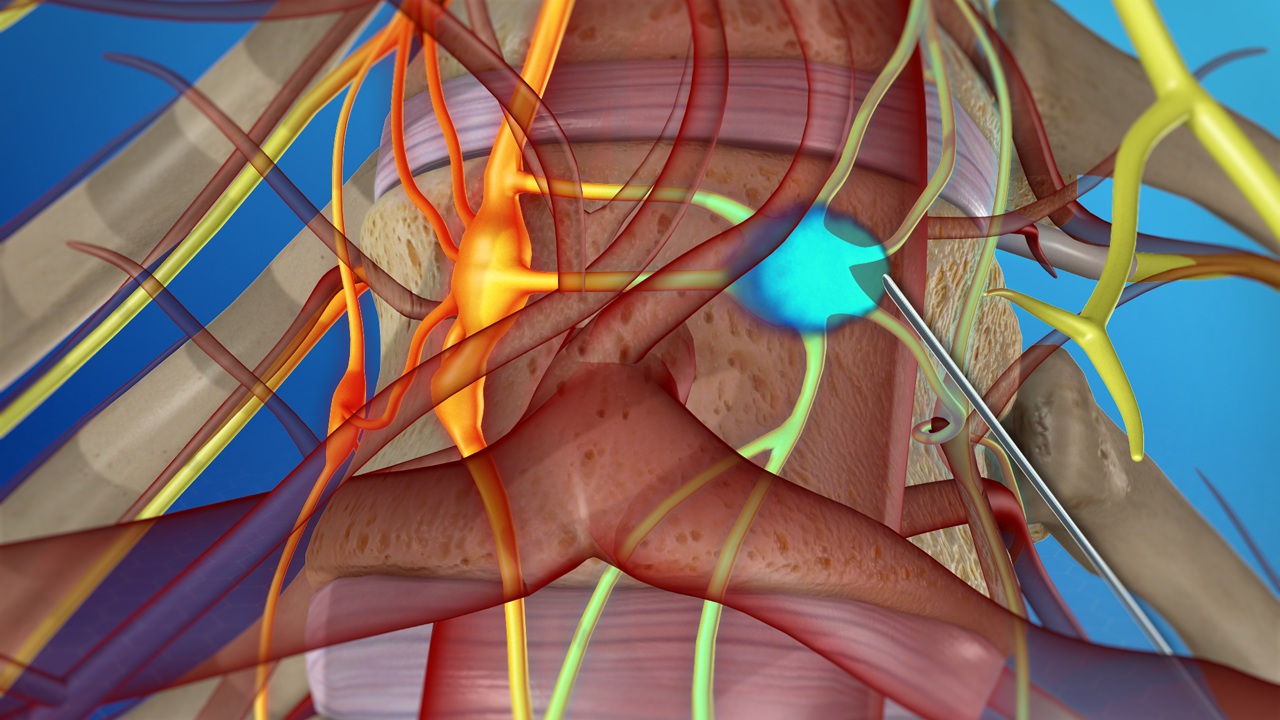
- In medical treatment for headache or migraine usually concentrate on medication for a long time, but one should opt for minimally invasive interventional pain management with sphenopalatine ganglia conventional or pulse radiofrequency treatment.it is a non-surgical treatment usually given by a qualified highly trained interventional pain physician. under fluoroscopic guidance, he localised the exact site and do the needful procedure.
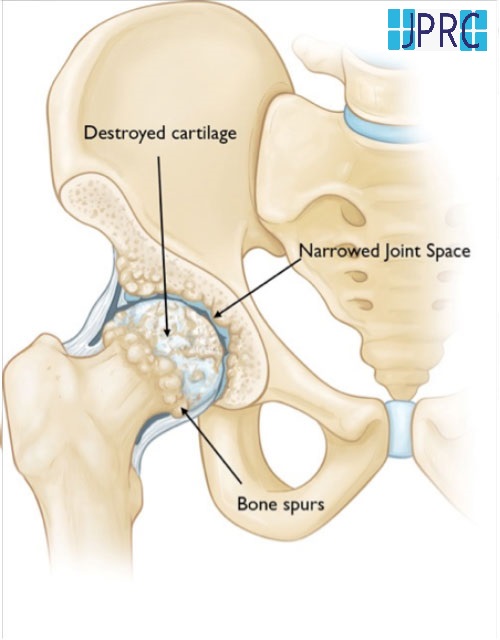
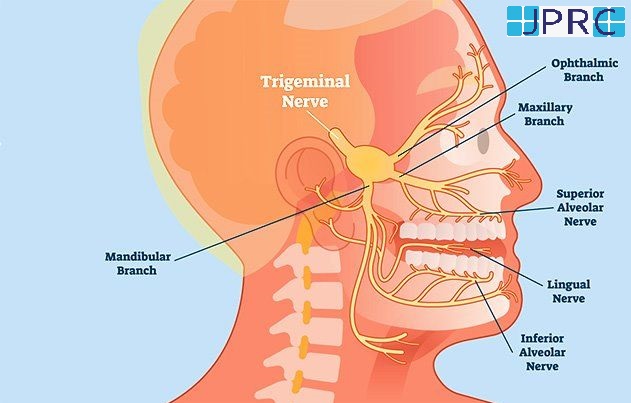
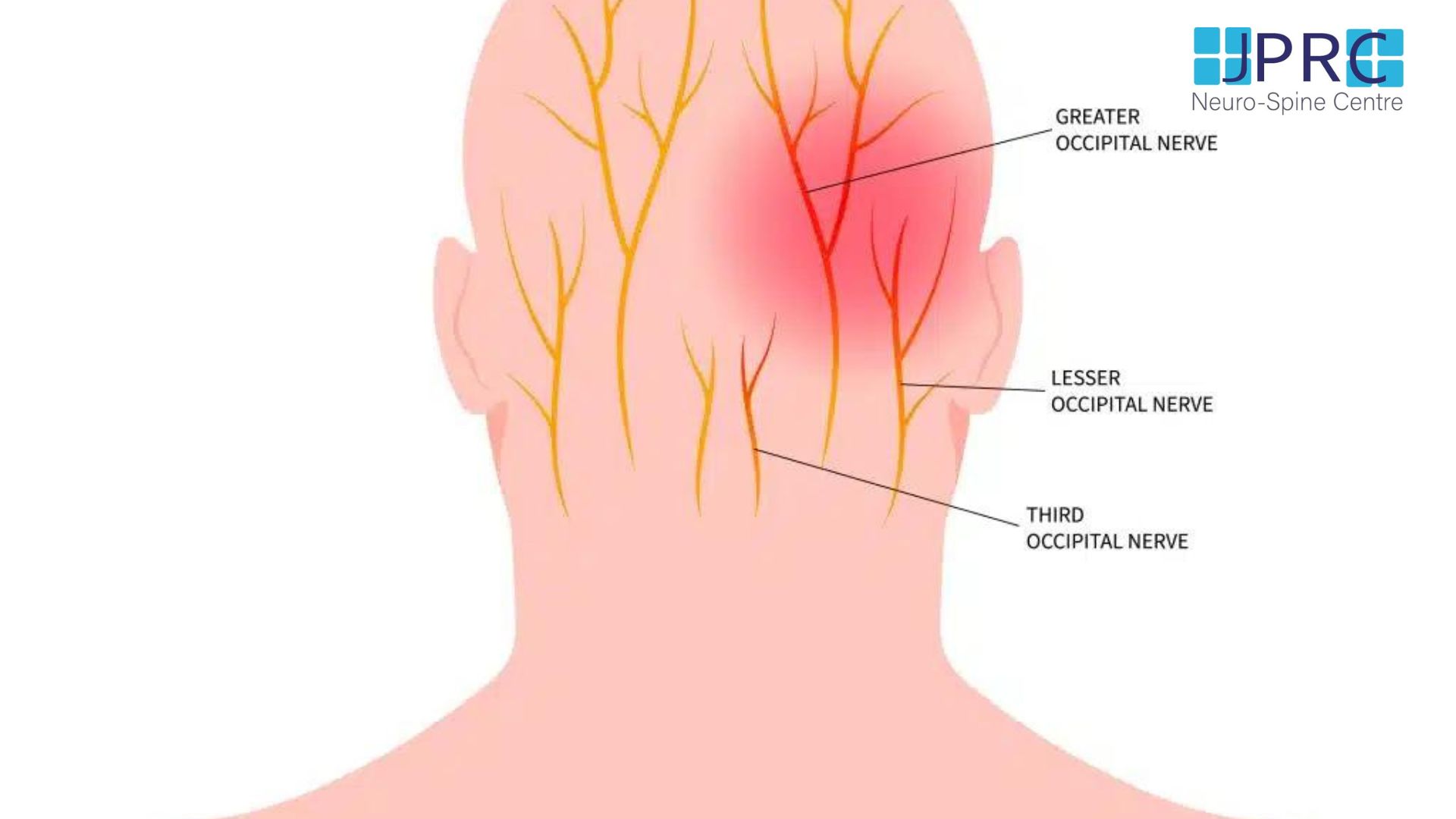
SPHENOPALATINE GANGLION:
It is a small collection of nerve cells and fibres located next to the mandible and behind the maxilla. It is carrying different kind of nerve cells and fibres: parasympathetic, sympathetic sensory and motor. Some of the nerves going through this ganglion are related to different kind of headaches and facial pain.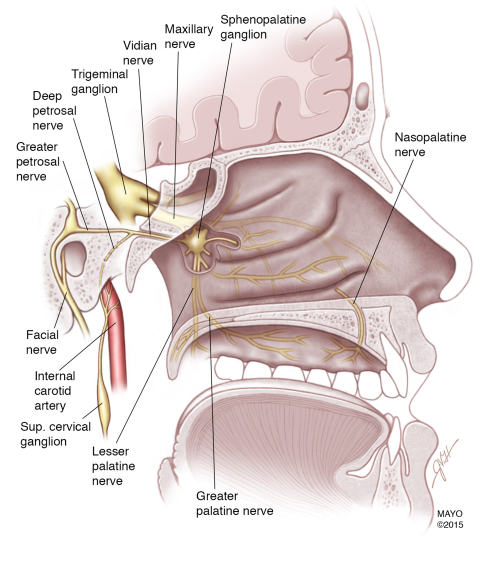
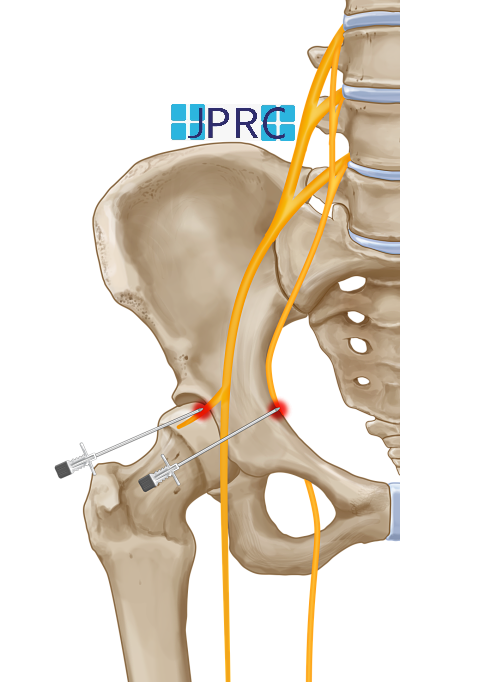
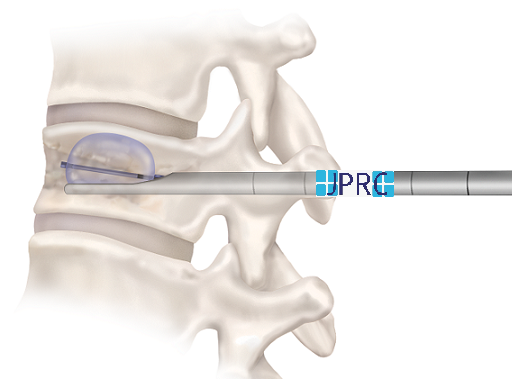
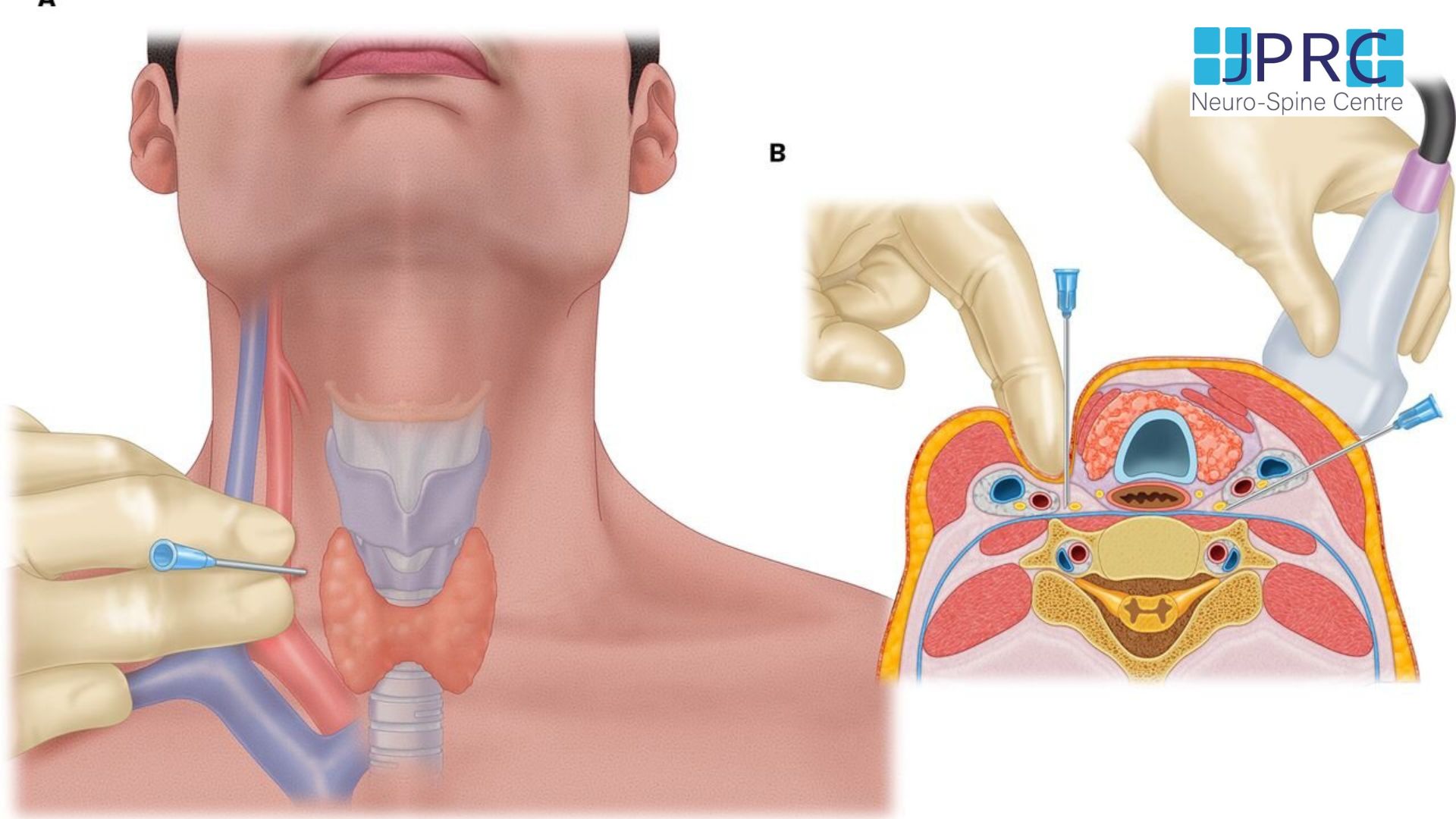
SPHENOPALATINE GANGLION BLOCK:
Block: A Sphenopalatine ganglion block is a short, minimally invasive procedure that is done using a local anaesthetic (+/- Steroids) to inhibit the signals going through those nerves and control the facial pain. It is effective in treating some acute and chronic facial and head pain. Also, it is considered a diagnostic tool to determine the point where pain signals can be interrupted.
A: With successful pain control after the block, long term pain relief can be achieved in some conditions by doing what so-called RadiFrequency Ablation to the same nerves. It is an electrical current produced by a radio wave that is used to heat a small area of nerve tissue, resulting in decreasing pain signals from that specific area. percutaneous radiofrequency ablation of the sphenopalatine ganglion is an extremely effective modality of treatment for patients with intractable chronic cluster headaches.
SPG BLOCKS HAVE BEEN REPORTED TO TREAT THE FOLLOWING CONDITIONS:
-
Cluster headache
- Migraine
- Trigeminal neuralgia
- Herpes zoster
- Paroxysmal hemicrania
- Cancer of the head or neck
- Atypical facial pain
- Complex regional pain syndrome (CRPS)
- Temporomandibular disorder
- Nasal contact point headache
- Vasomotor rhinitis




















































.jpg)










_Injection_Description_in_Hindi.jpg)














.jpg)









.jpg)




.jpg)
.jpg)
.jpg)






.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)








1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)









2.jpg)
3.jpg)



4.jpg)
1.jpg)
2.jpg)

5.jpg)
6.jpg)


7.jpg)
2.jpg)

8.jpg)

9.jpg)
3.jpg)

10.jpg)

11.jpg)


12.jpg)
4.jpg)