lumbar spondylosis
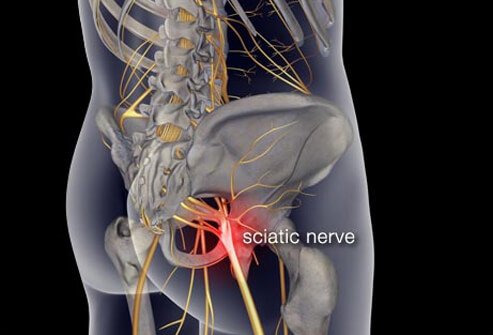
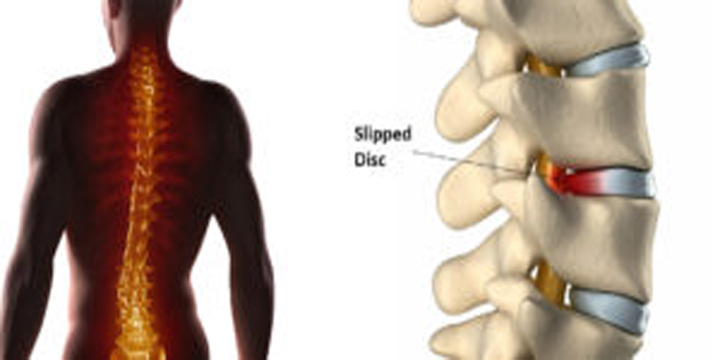
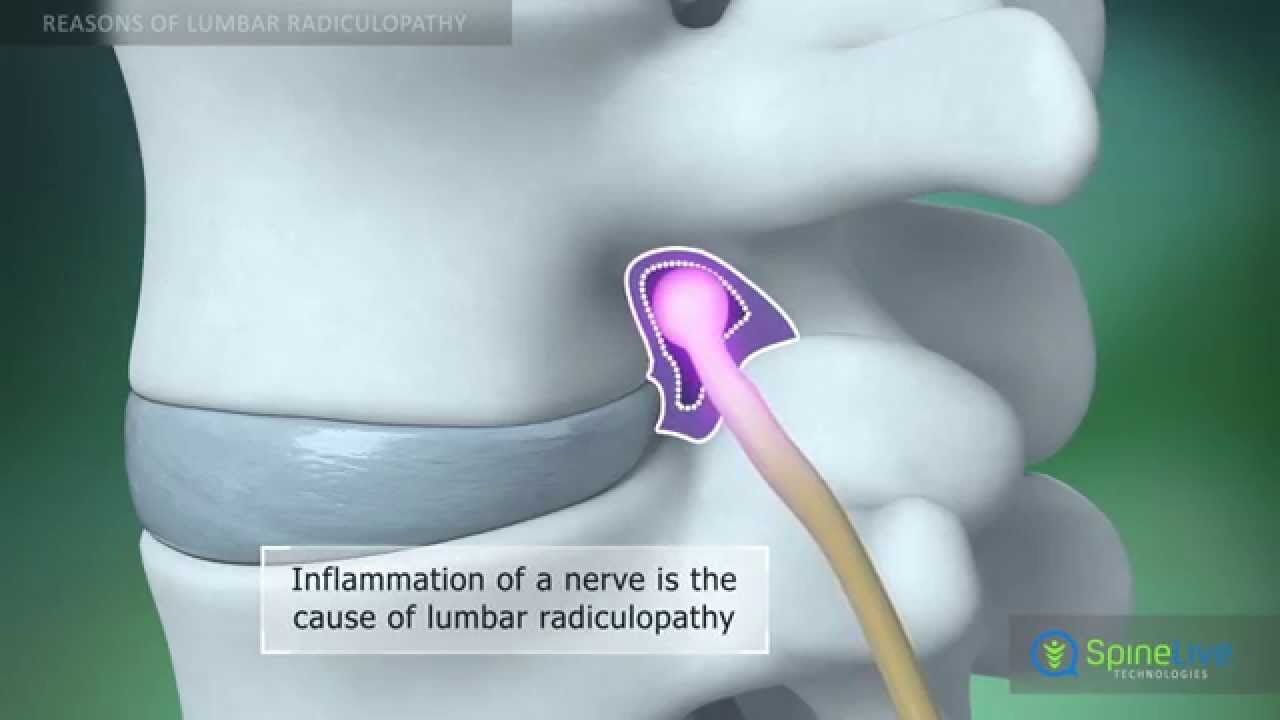
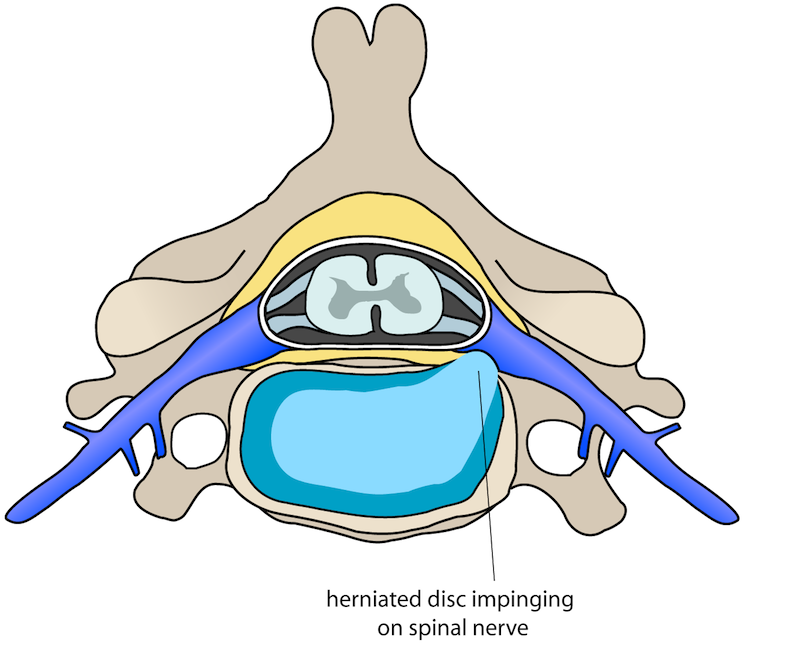
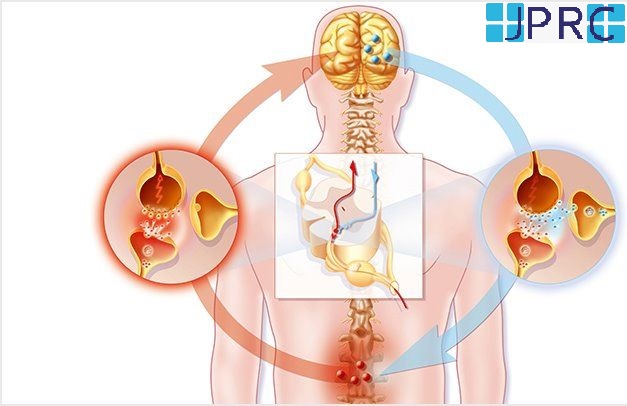
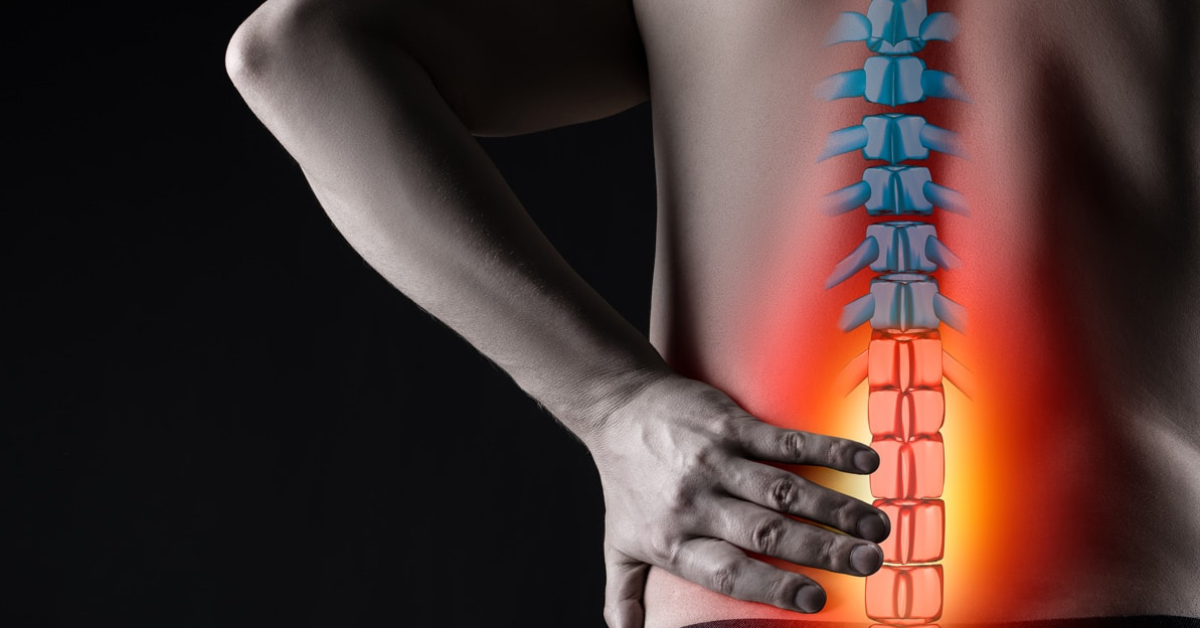
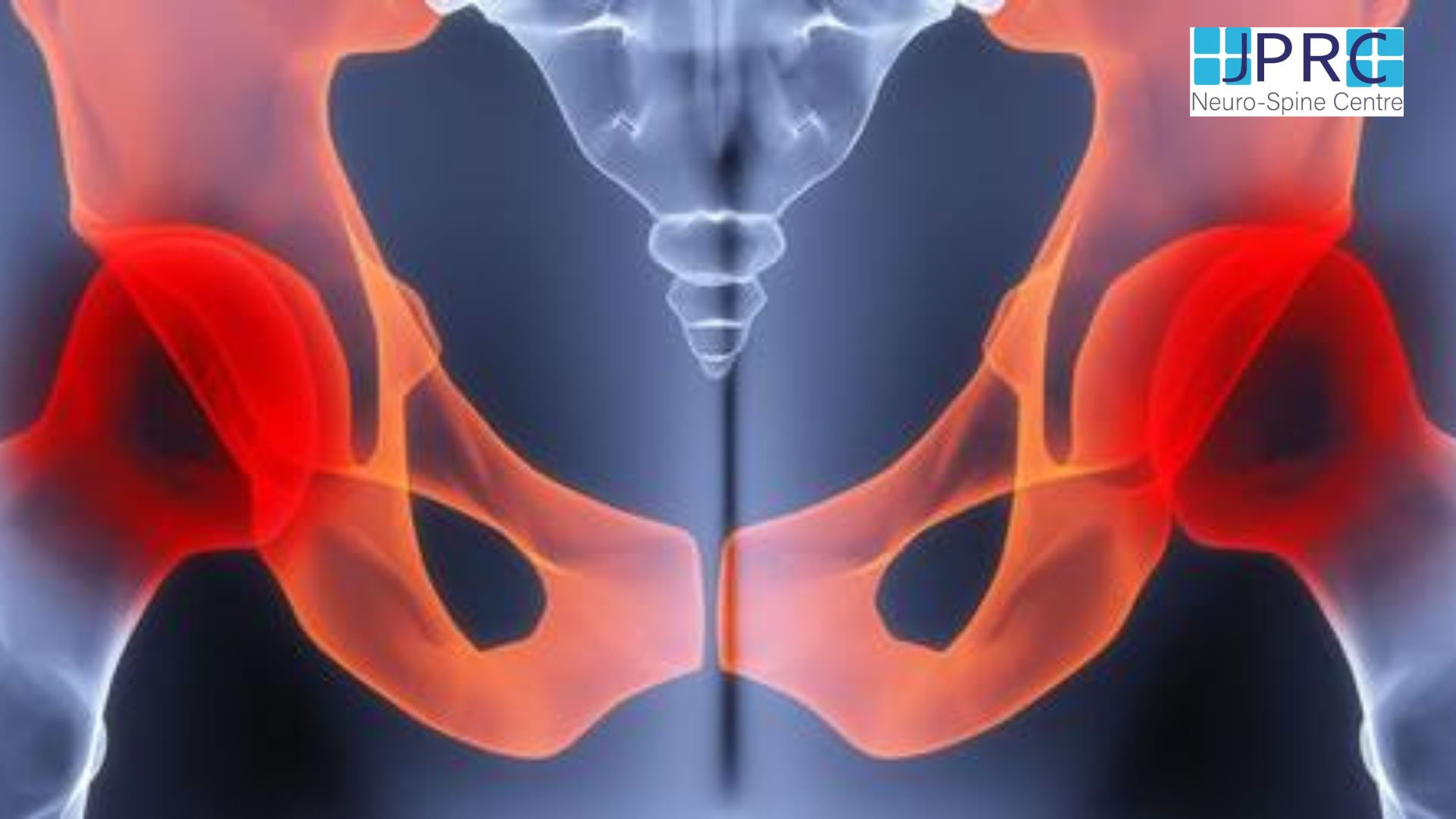
The clinical term refers to spondylosis that involves both the lumbar and the sacral spine. It occurs in the midline just below the lumbar spine (lower portion of the spine). Spondylosis is a medical term to describe the general deterioration[Degenerative] or age-related wear and tear that occurs in the spine. With advancing age, the spine is subjected to constant stress through bending and twisting movements, flexion, Rotation and most of the times associated with weight gain. This causes compression of the spinal components, like spinal nerves, theca, and spinal cord, which leads to the degradation of vertebral discs and joints.
While any portion of the spine may be affected by spondylosis, it occurs more commonly in the lowermost portion of the spine, where the lumbar vertebra meets the sacrum or the tailbone.at L5S1 level This is classified as lumbosacral spondylosis or L5-S1 spondylosis as it occurs between the last vertebra of the lumbar spine (L5) and the first vertebra of the sacral spine (S1). The lumbar spine largely supports and stabilizes the body by bearing most of the body weight. Therefore, the lumbar spine is subjected to most of the compression and resultant deterioration.
Symptoms of Lumbosacral Spondylosis
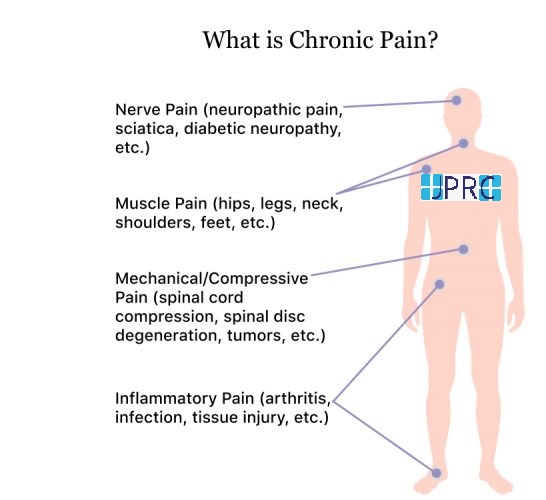
Lumbosacral spondylosis itself may not cause any symptoms, but it can lead to other conditions of the spine that cause back pain, stiffness, and limited range of motion. It generally affects people above 50 years of age, and most patients will have a mild to progressive form of spondylosis without any symptoms. But, if you experience low back pain, stiffness, and restricted mobility or inability to bend or move, you may need to consult your physician to find out whether you have progressive spondylosis.
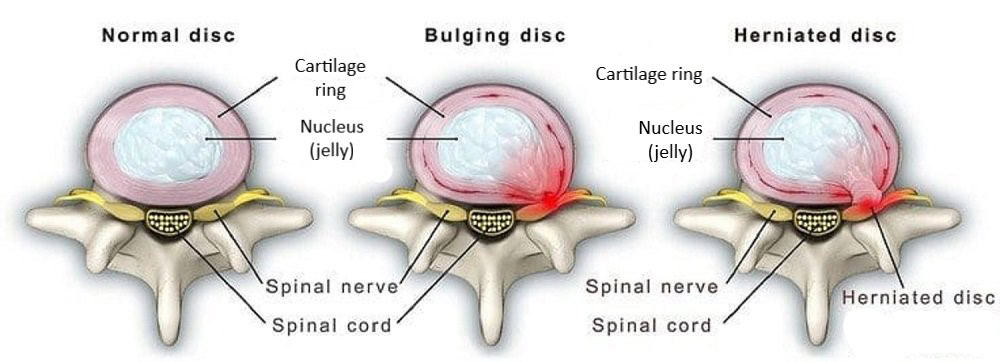
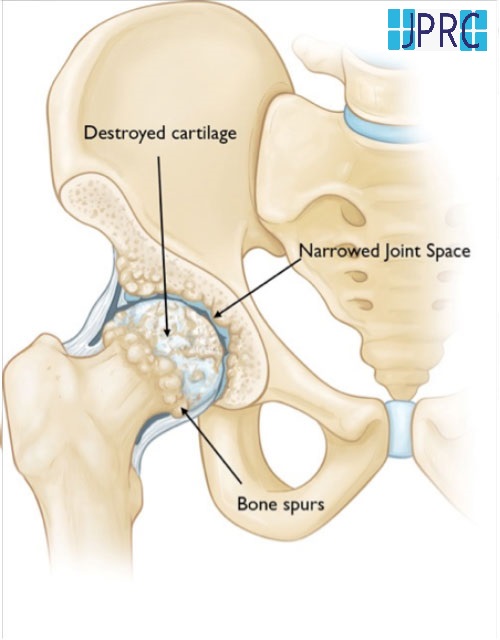
Spondylosis can cause further deterioration of the spine due to the development of other spine conditions such as stenosis, spondylolisthesis, Disc hernia, bone spurs, and degenerative disc disease. Usually, mild lumbar spondylosis does not cause additional spinal disorders. It is only when the spondylosis becomes progressive that there is a higher risk for the development of other spinal disorders.
Diagnosis of Lumbosacral Spondylosis
During your appointment, your physician will ask you questions regarding your pain and other symptoms along with your medical history. This allows your physician to determine the cause of pain and suggest the most suitable treatment plan.
The diagnosis of lumbosacral spondylosis is made through radiology tests namely, plain X-rays, Magnetic resonance imaging (MRI) scan, and Computed tomography (CT) scan. X-rays reveal bone spurs present on vertebral bodies in the spine, thickened facet joints, and narrow intervertebral disc spaces.
A magnetic resonance imaging (MRI) scan or computed tomography (CT) scan may be ordered to have a closer look at the spine. An MRI scan helps visualize the vertebrae, the Facet joints, the Nerves, and ligaments and can show a Pinched nerve. CT scan reveals Spinal stenosis or narrowing of the Spinal Canal.
An alternative option for spondylosis treatment
JPRC neuro-spine centre physicians recognize the potential benefits of alternative and complementary spondylosis treatment. There has been a great deal of evidence that techniques such as chiropractic therapy, deep tissue massage, and even herbal formulations can be beneficial in the management of spondylosis. You may be advised to try alternative medicine treatments before considering the surgical means of treatment by our doctors. Alternative medicine therapies include:
- Acupuncture: This ancient method of Chinese medicine involves pricking fine needles to various depths into certain specific areas of the body.
- Yoga: Yoga helps restore muscle strength in the core. In a way similar to physical therapy, Yoga strengthens the core muscles and helps maintain spine alignment, and slows down wear and tear. Certain yoga poses are designed to stretch the core and back muscles.
- Chiropractic Care: Chiropractic spinal manipulation can be of benefit to some people during the first month of pain. It is not recommended for patients with associated inflammatory arthritis of the spine, such as ankylosing spondylitis and rheumatoid arthritis, because of the risk of damage to the spinal cord.
- Therapeutic Massage: Massage, when done regularly in a proper way provides relief from chronic low back pain. Massage therapy is not suitable for people with conditions such as osteoporosis, open wounds, skin infections, deep vein thrombosis, and arthritis
Surgery for spondylosis
-
May be considered if the pain persists even after several weeks or months of conservative treatment.
-
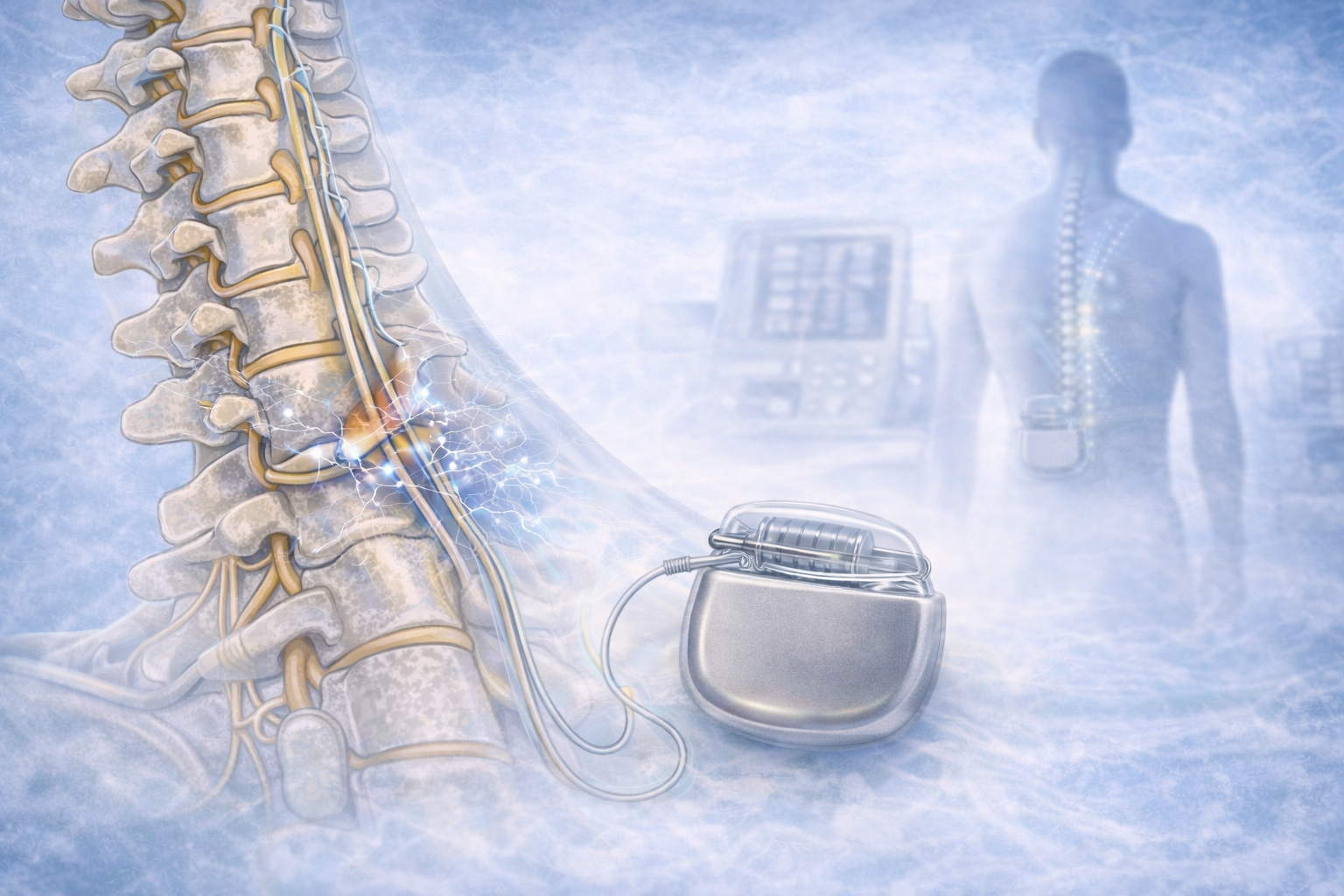
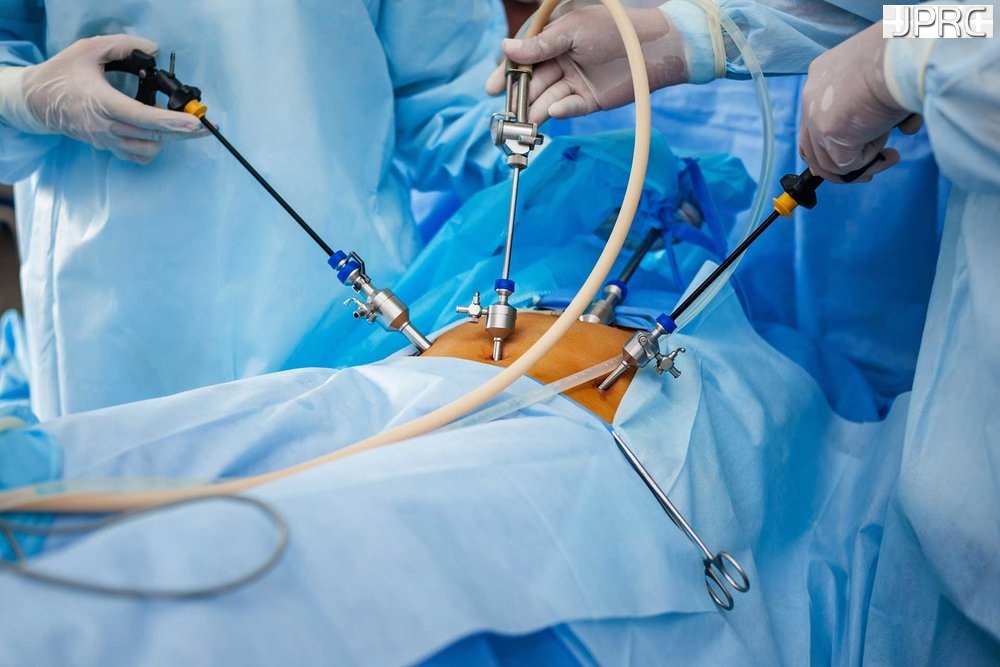
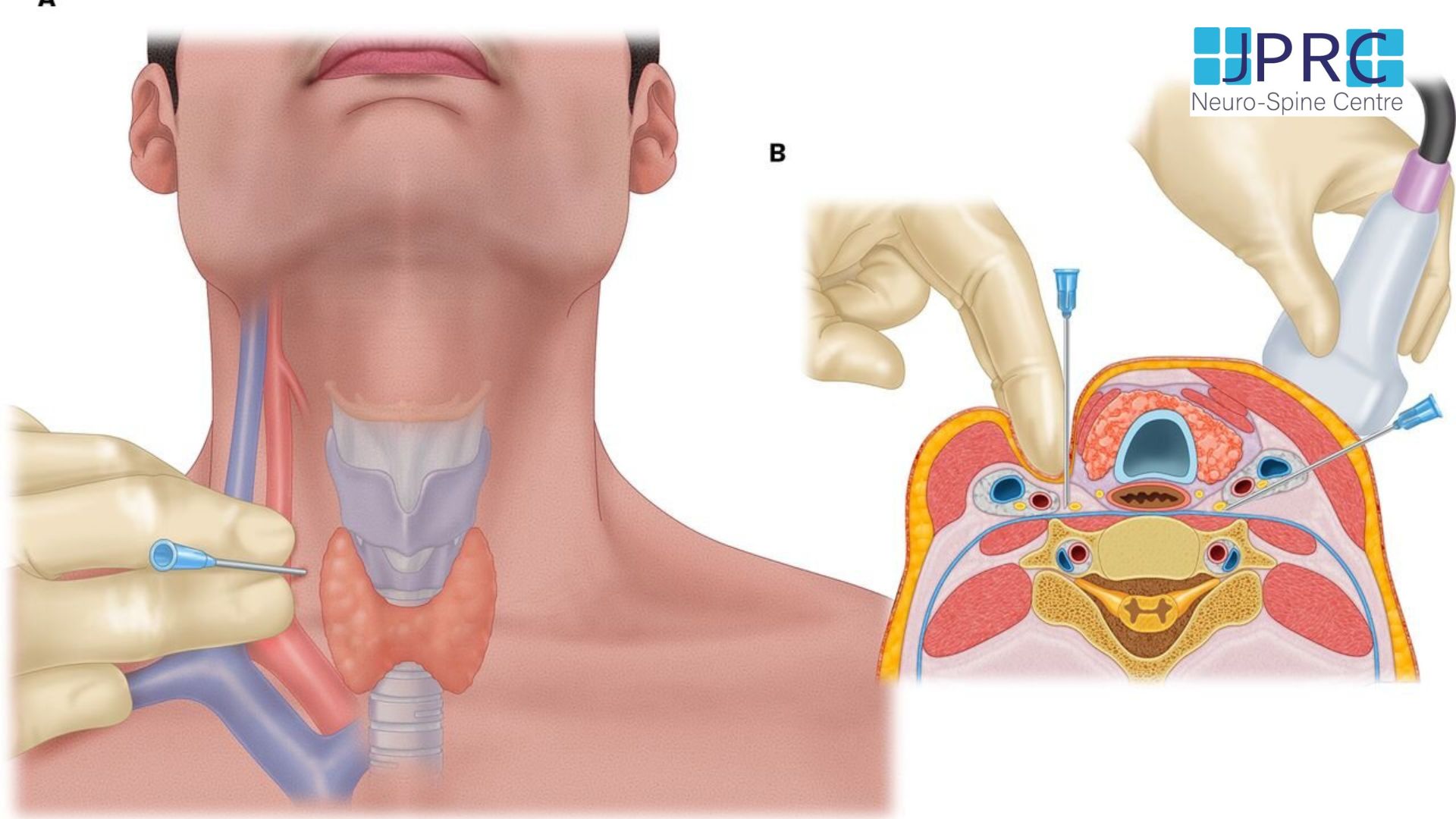
Spinal surgeons strive towards accomplishing their goal of providing sufficient pain relief with minimally invasive options. There are two surgical methods to treat spondylosis: Minimally invasive Stabilization and Minimally invasive Decompression. The choice of surgery is based on the severity of your condition or whether associated spinal conditions have developed because of spondylosis. This will be reviewed on an MRI or CT scan.
Minimally Invasive Stabilization Surgery
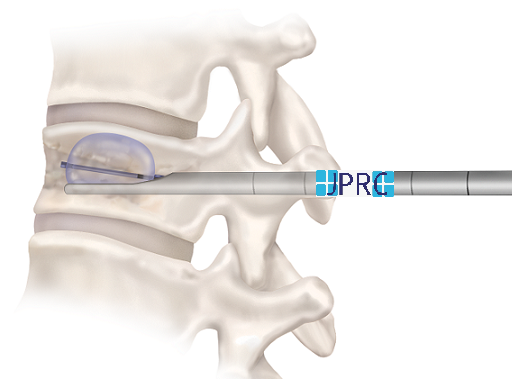
- The minimally invasive stabilization surgery provides a more precise alternative to traditional open back fusion surgery. The procedure involves the placement of a tiny cut in the back or side. Through this opening, the surgeon moves the surrounding muscles aside to avoid any tearing of the muscle tissue. With the muscles retracted, the surgeon removes the worn-out disc or vertebra and places an implant or bone. This will provide immediate stability to the spine and pain relief. The surgery is performed on an In-patient basis and you can return home on the next day of the surgery.
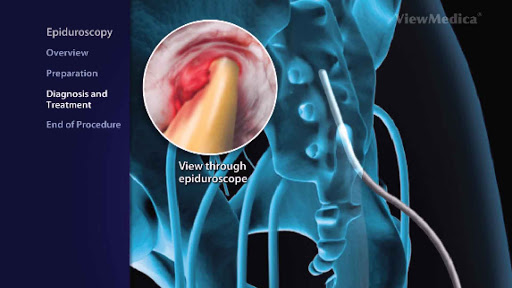
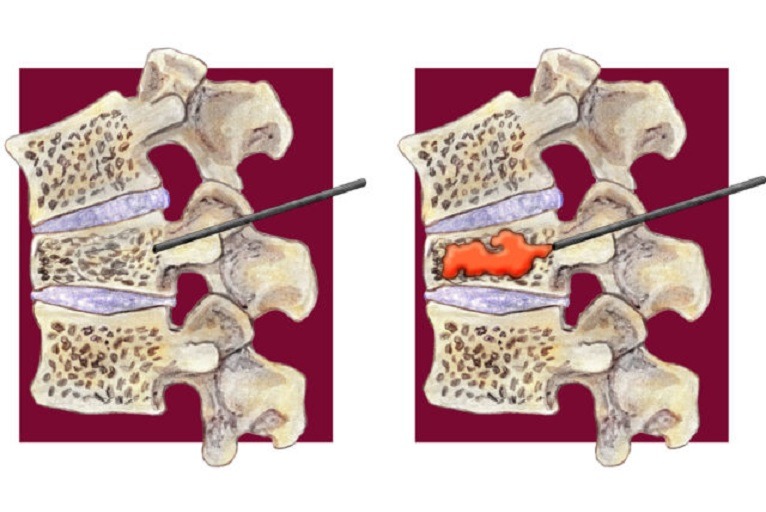
Minimally Invasive Decompression Surgery
-
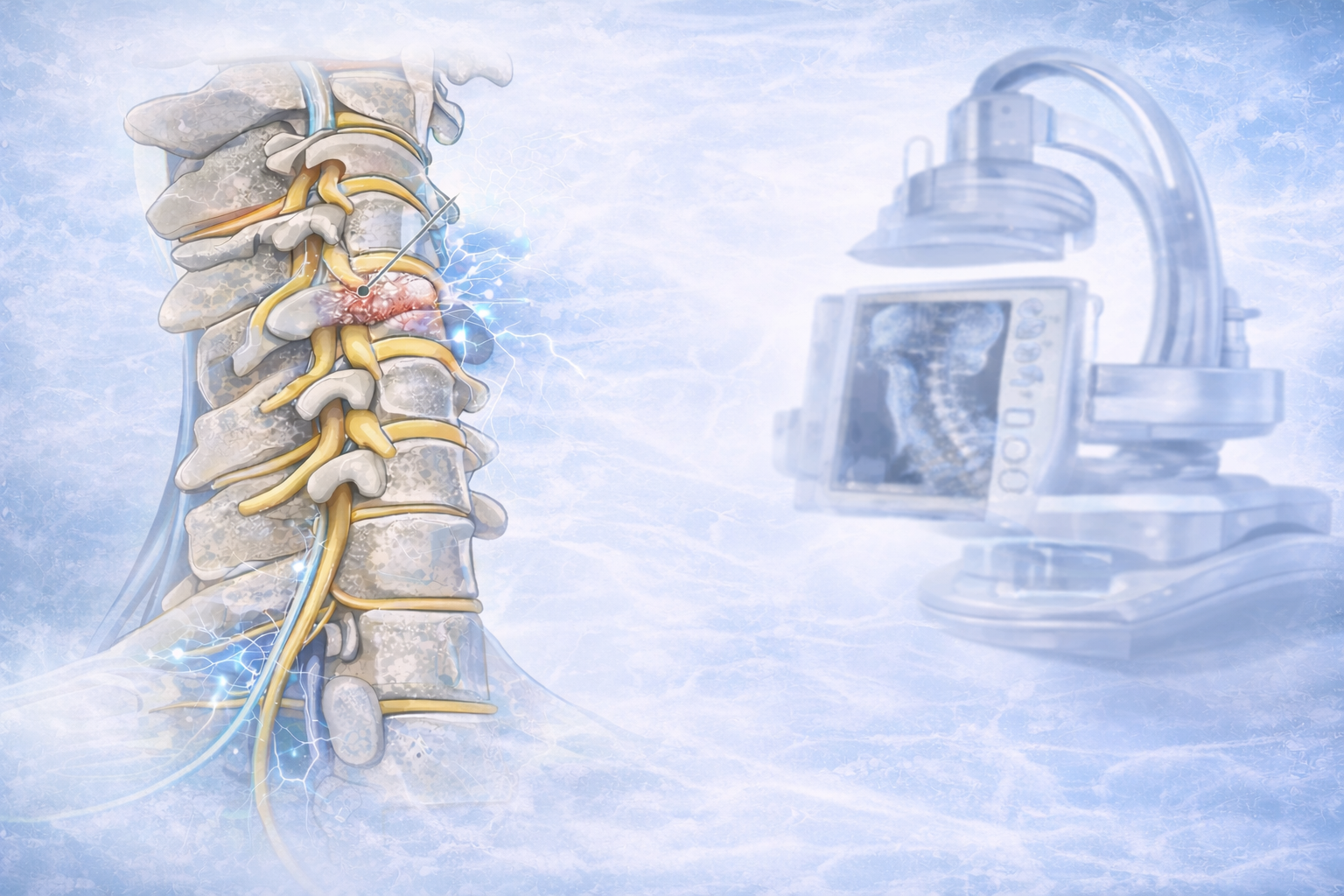
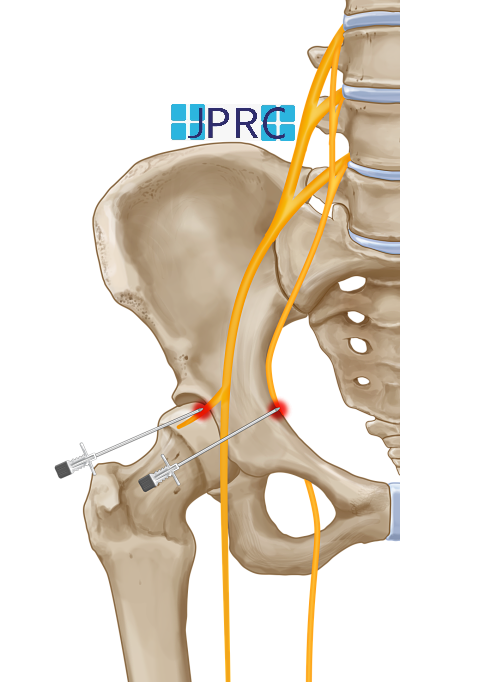
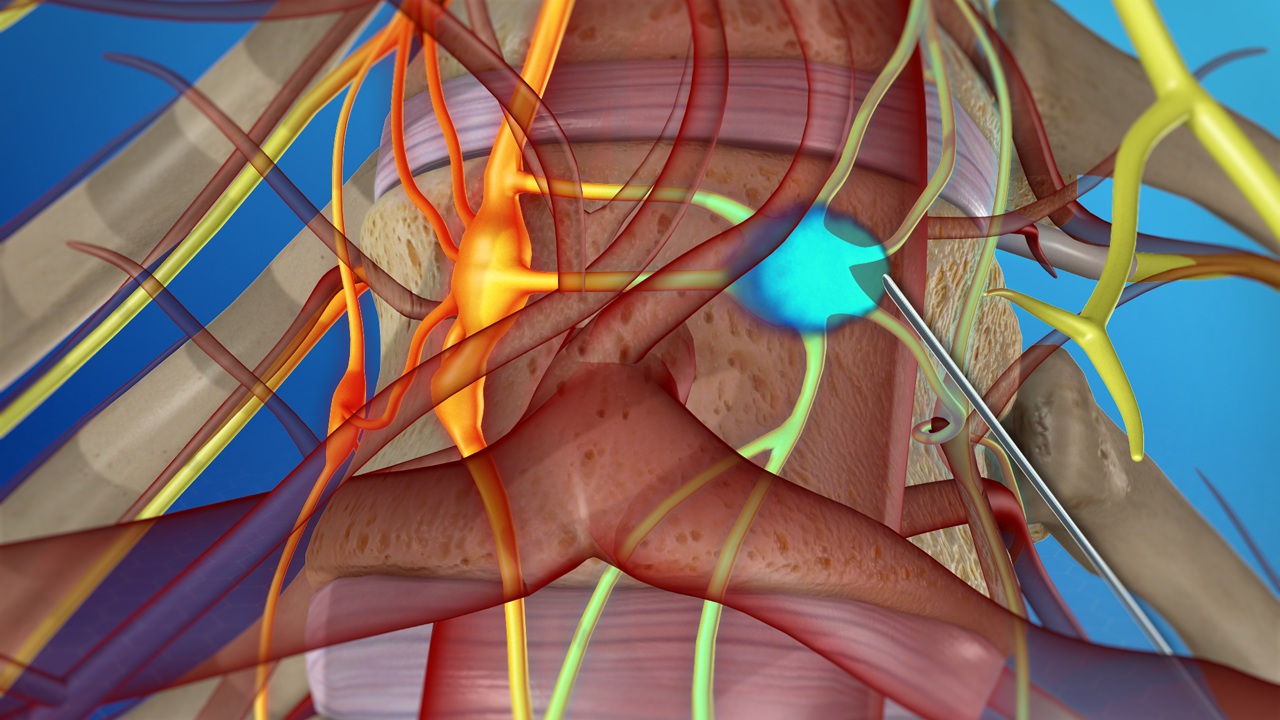
This surgery is generally performed when spondylosis leads to nerve compression along the spinal cord that causes local and radiating pain. The minimally invasive techniques allow the surgeon to enter the affected portion of the spine through a tiny, less than 1-inch long incision. The surgeon will remove the part of the bone or disc that compresses a spinal nerve. This is an outpatient procedure and you can leave the hospital on the same day of your surgery. The Spinal nerve Decompression techniques include – Foraminotomy, Laminotomy, Discectomy, and Facet thermal Ablation to weaken the painful nerves in the facet joint. Small cameras are used to find out the cause of the Nerve compression and the problem is tackled without destabilizing the spine.
Advantages of Minimally Invasive Spine Surgery
- Minimally invasive procedures are performed on an outpatient basis or inpatient basis
- Small incision, usually less than 1-inch in length
- Surrounding musculature and soft tissue remain intact
- Shorter recovery span 24-72 hours
- Greater patient satisfaction
- Reduced risk of postoperative complications such as infection, and pain




















































.jpg)










_Injection_Description_in_Hindi.jpg)














.jpg)









.jpg)




.jpg)
.jpg)
.jpg)






.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)








1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)
1.jpg)









2.jpg)
3.jpg)



4.jpg)
1.jpg)
2.jpg)

5.jpg)
6.jpg)


7.jpg)
2.jpg)

8.jpg)

9.jpg)
3.jpg)

10.jpg)

11.jpg)


12.jpg)
4.jpg)