Discography
Discography was first described in 1948 as an investigative technique for herniated nucleus pulposus. Since that time, new imaging techniques that are more appropriate for this diagnosis have been developed. Discography is currently used to determine whether the disk is the source of pain in patients with predominantly axial back or neck pain.[1]
During discography, contrast medium is injected into the disk and the patient’s response to the injection is noted; provocation of pain that is similar to the patient’s existing back or neck pain suggests that the disk might the source of the pain. Computed tomography (CT) is usually performed after discography to assess anatomical changes in the disk and to demonstrate intradiscal clefts and radial tears.
Early studies suggested that discography had a low specificity, but more recent studies have failed to induce pain in asymptomatic controls, suggesting that discography has utility in identifying patients with discogenic pain. Pain reproduction during discography in symptomatic individuals is variable, with a lower incidence of pain reproduction in patients with disk degeneration than in those with posterior tears of the anulus fibrosus or significant disk bulges.
Controlled clinical trials of discography are lacking, and a standard against which to compare is elusive. When comparing outcomes of fusion procedures, lumbar discography is sensitive but lacks specificity. See the images below.
Lateral view.

Lateral view.

Anteroposterior view.
Relevant Anatomy
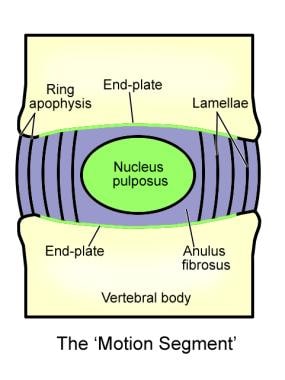
Discs form the main connection between vertebrae. Their size varies depending on the adjacent vertebrae size and comprises approximately one quarter the length of the vertebral column.
These disks are composed of 4 parts: the nucleus pulposus in the middle, the annulus fibrosis surrounding the nucleus, and 2 end plates that are attached to the adjacent vertebral bodies (see the image below). They serve as force dissipators, transmitting compressive loads throughout a range of motion. The disks are thicker anteriorly and therefore contribute to normal cervical lordosis.
Indications
Discography should be performed only if adequate attempts at conservative therapy and noninvasive diagnostic tests, such as MRI, have failed to reveal the etiology of back pain.
Specific indications for discography include the following:
-
Persistent, severe symptoms when other diagnostic tests have failed to clearly confirm a suspected disk as a source of the pain
-
Evaluation of abnormal disks or recurrent pain from a previously operated disk or lateral disk herniation
-
Assessment of patients in whom surgery has failed, to determine whether pseudoarthrosis or a symptomatic disk in a posteriorly viewed segment could be the source of pain
-
Assessment of disks prior to fusion to determine whether the disks of the proposed fusion segment are symptomatic and whether the disks adjacent to this segment can support a fusion
-
Assessment of candidates for minimally invasive surgery who have a confirmed disk herniation
-
Discography Procedure Technique
-
Prophylactic antibiotics should be considered.
-
Double-needle technique always should be used.
-
The injection should be performed with water-soluble contrast medium.
-
Accurate needle placement is required to avoid annular injections, which could produce false-positive results.
-
Injection against the vertebral end plate can cause a false-positive response.
-
Discography should be followed by CT scanning.
-
The information recorded should include the following:
- Resistance to the injection (ie, end point)
- Amount of contrast material injected (ie, maximum volume)
- Volume at which the patient experienced pain (ie, pain volume)
- Pattern of dye distribution (eg, diffusion, location of fissure, extravasation, herniations, Schmorl nodule)
- Pressure at which patient experienced “pressure sensation”
- Pressure at which patient experienced “pain”
- Pain response (ie, location, character, distribution, intensity, and concordance or discordance with the patient’s typical pain and pain pattern)
- Pain intensity recorded on a 0-10 scale
Interpretation
See the list below:
-
Very careful attention should be paid to interpreting the pain response during the injection of each disk, including whether the pain is similar to or exactly like the symptoms for which the patient seeks relief. The location of the pain and its intensity should be noted.
-
Pain at low pressures is most likely due to chemical irritation. Low resistance generally is associated with a tear through the outer annulus. Pain at high pressures may be due to mechanical irritation, end-plate deflection, or stimulation of pressure receptors.
-
Generally, if a large volume of contrast can be injected, the disk is degenerated or has a fissure extending through the outer annular wall.
-
The specificity of discography findings could be increased if CT scanning findings are correlated. Annular disruption reaching the outer annulus fibrosus is a key factor in pain generation. Disk morphology, including annular disruptions extending beyond the outer annulus, may permit increased discography specificity. [3]
Dallas classification of discography results
See the list below:
-
Type 1: The discogram is normal manometrically, volumetrically, and radiographically and produced no pain. The discogram/CT scan showed contrast to be located centrally in the axial and sagittal projections. See the image below.
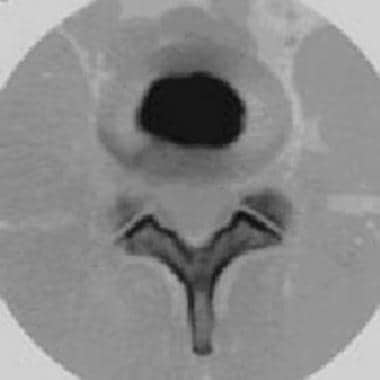
Postdiscography CT scan showing normal disk contour.
-
Type 2: This is identical to type 1 except that it is positive for reproduction of pain.
-
Type 3: Annular tears lead to a radial fissure. This group is subdivided further into types 3a (ie, posterior radial fissure), 3b (ie, fissure radiates posterolateral), and 3c (ie, fissure extends lateral to a line drawn from the center of the disk tangential to the lateral border of the superior articulating process).
-
Type 4: Once the radial fissure reaches the periphery of the anulus fibrosus, nuclear material may protrude, causing the outer annulus to bulge.
-
Type 5: When the outer annular fibers rupture, nuclear material may extrude beneath the posterior longitudinal ligament and come in direct contact with either the dura or a nerve root.
-
Type 6: When the extruded fragment is no longer in continuity with the interspace, it is said to be sequestrated. Manometrically, volumetrically, and radiographically, the discograms are always abnormal. Familiar pain may be reproduced only if enough pressure is generated against the free fragment to cause stimulation of the pain-sensitive structures.
-
Type 7: The end stage of this degeneration is internal disk disruption, characterized by multiple annular tears. The discograms are abnormal manometrically and volumetrically, and familiar pain may or may not be reproduced. Radiographically, the contrast usually fills the entire interspace in a chaotic fashion. The discogram/CT scan shows contrast extravasation throughout multiple annular tears. See the image below.

Postdiscography CT scan showing some abnormal dye spread.
-
Neck Pain Treatment non surgical
Hip Joint pain radio frequency treatment
Minimal Invasive Spine Surgery
